
Preeclampsia
Preeclampsia (pre-e-CLAMP-si-a) is one of the most common birth complications affecting women in the United States. In fact, one out of every 20 women develop it. In the past two decades, the rate of preeclampsia in the United States has increased by more than 25%. It is considered one of the leading causes of maternal death and fetal illness and death. It is a problem that affects women around the world.
Healthcare providers should discuss preeclampsia with women who are pregnant, or who are planning to become pregnant. Recognizing the symptoms and getting immediate medical care is important to reduce the risk of complications, birth injuries and death. Some cases of severe preeclampsia are life-threatening, and often, the disease is called a “silent killer.”
If someone you love has symptoms of preeclampsia, don’t wait to get medical help.
What is Preeclampsia?
Preeclampsia occurs when there is a rise in blood pressure and protein in the urine during pregnancy. It generally starts around the 20th week of pregnancy, and can continue until the baby is born. There are also cases of preeclampsia developing just after birth, known as postpartum preeclampsia, but these are less common. Preeclampsia may cause blood platelets to drop, and may cause organ damage. In some cases, preeclampsia can escalate to include fluid in the lungs, kidney or liver failure, seizures and/or visual impairment. The most severe cases develop into eclampsia or HELLP syndrome.
Many women have heard the terms “toxemia” and “pregnancy induced hypertension” (PIH). You should know that these terms are outdated and medical experts no longer utilize them. Instead, the ACOG and the Preeclampsia Foundation focus on two forms of preeclampsia:
- Preeclampsia-eclampsia
- Preeclampsia superimposed on chronic hypertension
There are also two other pregnancy-related disorders that affect blood pressure:
- Chronic hypertension (may or may not be diagnosed before pregnancy, but is not pregnancy related)
- Gestational hypertension (high blood pressure that develops and increases during pregnancy; may lead to preeclampsia)
What is Eclampsia?
Preeclampsia-eclampsia is one of the more common manifestations of the disease. When preeclampsia escalates, it can turn into eclampsia, which means the mother is also experiencing seizures. In developed nations like the U.S., eclampsia can almost always be prevented with timely diagnosis and treatment of preeclampsia. Delays in diagnosis or treatment can lead to serious problems like coma, brain damage and maternal or fetal death.
What Causes Preeclampsia?
The causes of preeclampsia involve several factors. Experts generally believe that it begins in the placenta. The placenta is the organ that grows during pregnancy and provides the majority of nutrients for the fetus. Early in pregnancy, new blood vessels develop and eventually send blood and nutrients to the placenta.
In women who have preeclampsia, the blood vessels don’t form or function as they should. They tend to be more narrow and they react differently to hormones. These reactions can limit the amount of blood that flows to the baby. This puts the baby at risk for intrauterine growth restriction, oxygen deprivation and a lack of nutrients. Abnormal development of the placenta may be caused by:
- Lack of blood flow to the uterus
- Damaged blood vessels
- Immune system problems
- Genetics
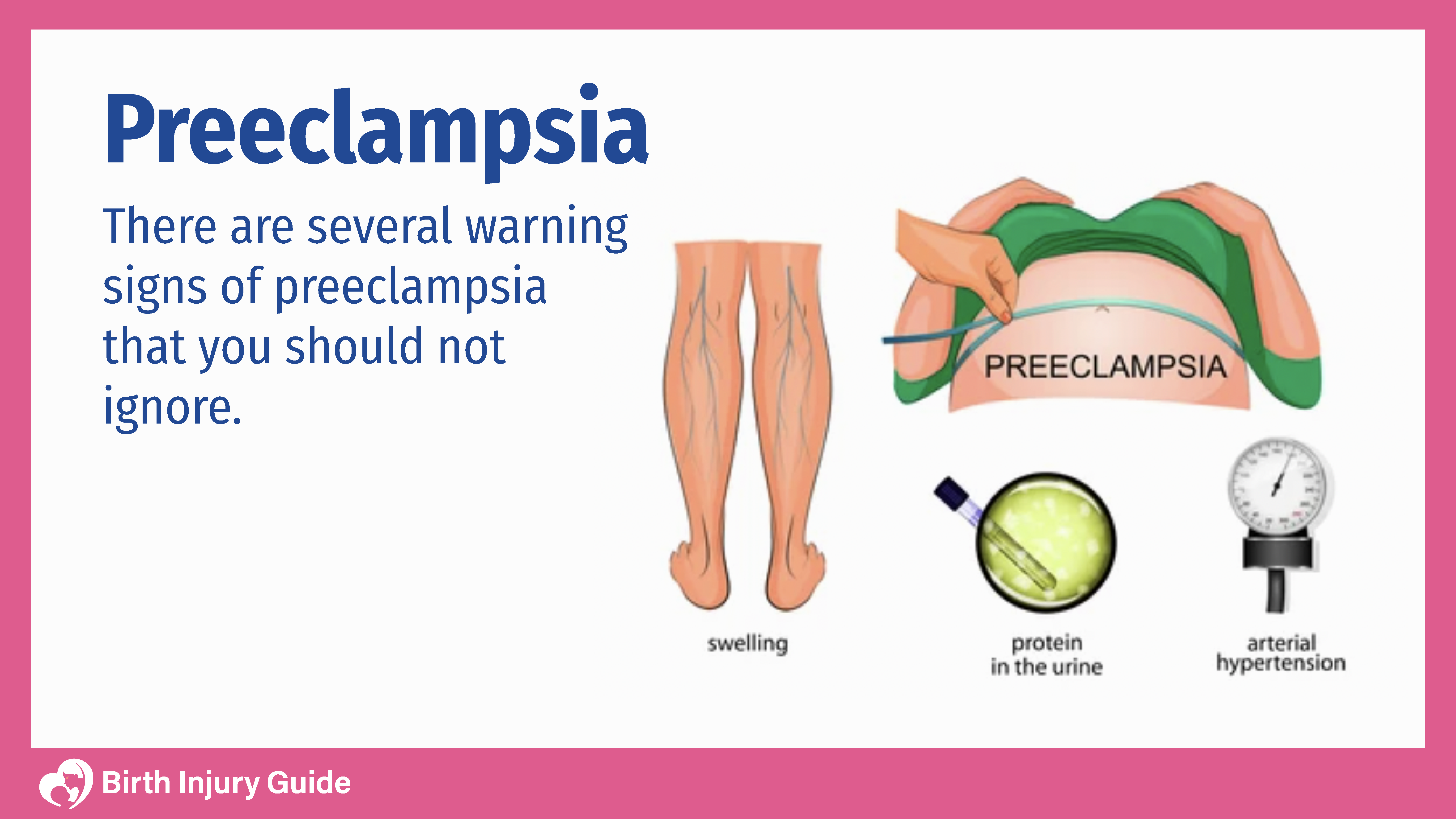
Preeclampsia Symptoms
There are a number of symptoms associated with preeclampsia, yet in some instances, it will develop without the mother noticing any symptoms at all. Often times, high blood pressure is noted during a prenatal visit or routine blood pressure check. Pregnant women should be aware of what their normal blood pressure level is, and when they should worry. Consequently, it’s imperative to monitor blood pressure throughout pregnancy. The Mayo Clinic suggests that blood pressure that’s 140/90 or higher is abnormal.
Women who have preeclampsia may notice some symptoms that are uncomfortable or unusual. Sometimes, women attribute these symptoms to pregnancy. After all, pregnancy can be uncomfortable and women often experience changes in their body that they aren’t familiar with. Furthermore, women are often not advised of the risks of conditions like preeclampsia. Sadly, many women do not realize that the symptoms they are experiencing are those of preeclampsia. This can lead to a delay in diagnosis and treatment, which can be life-threatening.
Symptoms that women should be aware of include:
- Shortness of breath
- Abdominal pain
- Edema (swelling in the hands and face)
- Nausea, sometimes accompanied with vomiting
- Poor liver function
- Excessive protein in the urine
- Pain below the rib cage
- Severe headaches
- Blurry vision
- Visual spots or auras
Pregnant women who experience these symptoms should talk to their healthcare provider immediately. Your doctor will likely want to run some tests and monitor your blood pressure for a period of time. You may also be ordered to bed rest, or may even be hospitalized if your doctor suspects severe preeclampsia.
Risk Factors
There are quite a few risk factors that heighten a pregnant woman’s risk of developing this condition, including:
- Age: Women who get pregnant at age 35 or older are more at risk for preeclampsia, as are women who are incredibly young (younger than 20).
- Race: Rates of preeclampsia are higher among Black women than women of any other race.
- History: Previous pregnancies with preeclampsia significantly increase the risk for additional pregnancies with preeclampsia.
- First Pregnancy: Women are most at risk for preeclampsia during their first pregnancy.
- Maternal Obesity: The risk of gestational hypertension during pregnancy is greater if the mother is obese.
- Multiples: Carrying more than one infant increases the risk of premature birth, low birth weight and preeclampsia.
- Paternity: Any first pregnancy with new paternity than previous pregnancies increases the risk of preeclampsia.
- History: Certain medical conditions can increase the risk of hypertensive disorders, such as chronic high blood pressure, Type 1 or 2 diabetes, kidney disease, blood clotting disorders or lupus.
- In Vitro: If your baby was conceived using in vitro fertilization, then your risk of developing preeclampsia is higher.
- Interval: Your risk of preeclampsia is higher if you have pregnancies less than two years apart, or more than 10 years apart.
Complications of Preeclampsia
When preeclampsia occurs, both mother and infant are at risk for serious health complications. Many women with preeclampsia are able to complete their pregnancies and deliver healthy babies. Sadly, many others feel the full effects of preeclampsia and related disorders and complications. Timely diagnosis and treatment is the key to helping mom and baby be healthy. However, without timely diagnosis and treatment, serious complications can develop including:
Placental Abruption
Placental abruption occurs when the placenta separates from the inner wall of the uterus before childbirth. This can cause heavy bleeding, and can be life-threatening without immediate diagnosis and treatment.
Placental Insufficiency
Placental insufficiency may mean you have a small placenta, or that your placenta is not functioning properly. When the placenta does not function properly, the infant may not get the blood, oxygen and nutrient supply that they need to be healthy. This can lead to many additional health risks. Insufficient blood flow to the placenta can result in oxygen deprivation at birth.
Eclampsia
Eclampsia is preeclampsia accompanied with seizures. It is very difficult to determine which cases of preeclampsia will escalate, so doctors must be diligent in monitoring mothers. Eclampsia often develops without any warning or symptoms. It can quickly become emergent or life-threatening.
HELLP Syndrome
HELLP stands for hemolysis, elevated liver enzymes, and low platelets. This is a serious condition that can develop in women with preeclampsia. More information about HELLP is discussed in the next section.
Cardiovascular Disease
Women who have preeclampsia are at an increased risk of developing heart and blood vessel diseases later in life. The risk is greatest among women who have had more than one pregnancy with preeclampsia, as well as women who delivered prematurely. Experts suggest some of the risk can be mitigated by living a healthy and active lifestyle and avoiding smoking.
Organ Damage
Preeclampsia can cause organ damage that may be permanent. Women often experience damage to the kidneys, liver, heart, lungs, and eyes. If there are seizures or stroke, then there may also be brain damage. Other organs may suffer damage due to preeclampsia, but this damage often depends on how ill the mother was.
What is HELLP Syndrome?
HELLP syndrome is one of the most severe types of preeclampsia. It occurs in around 5-12% of preeclampsia patients. HELLP is the acronym for hemolysis, elevated liver enzymes, and lowered platelets. HELLP syndrome doesn’t always include the symptoms of preeclampsia – protein in the urine or high blood pressure. The symptoms can easily be mistaken for the flu, glass bladder issues or even acute hepatitis.
HELLP syndrome is an incredible risk for women with preeclampsia. The mortality rate is as high as 30% even here in the U.S. Globally, it is considered a leading cause of maternal death. Women who think they may have preeclampsia or HELLP syndrome should get medical help right away. Pregnant women should contact their doctor if they experiencing any of the following:
- Severe headache
- Nausea and/or vomiting
- Abdominal or chest tenderness (upper right side)
- Shoulder pain when breathing
- Vaginal bleeding
- Visual disturbances (auras, spots, etc.)
- Swelling (edema)
It is imperative that someone with HELLP syndrome gets help immediately. Severe illness can develop quickly, including liver rupture or brain hemorrhage. Severe complications like these can be prevented if preeclampsia and/or HELLP are caught quickly and treated immediately.
The only treatment for HELLP syndrome is to deliver the baby. Sometimes, there is time for doctors to administer corticosteroids over a period of time to help the baby’s lungs develop properly. This is common when the pregnancy is not close to full-term. Sometimes, women will receive blood transfusions also, including blood, plasma and platelets. Depending on how far along the pregnancy is and the health of mom and baby, a c-section may be the best option to deliver the baby and start treatment for the mother.
How is Preeclampsia Diagnosed?
Historically, a preeclampsia diagnosis was based on high blood pressure and the presence of protein in the urine (proteinuria). However, in recent years, the guidelines from the American College of Obstetrics and Gynecologists (ACOG) has changed. Now, high levels of protein are not necessary in order for a diagnosis to be made. Research shows that organ damage can occur with preeclampsia without protein in the urine. Furthermore, the level of protein in the urine does not equate with how severe the disease is or how it will progress.
Now, to diagnose preeclampsia, doctors look at persistent high blood pressure during pregnancy or during the early postpartum period. High blood pressure that is accompanied by protein in the urine OR low blood platelets, organ dysfunction or signs of seizures warrants a preeclampsia diagnosis. High blood pressure is considered anything over 140/90. A single high blood pressure reading does not mean that you have preeclampsia. Doctors will take your blood pressure more than once to see if your readings go up or down, or remain consistently high. If you have more than one high reading in a four-hour period, your doctor may perform some tests to see if you have other signs of preeclampsia.
Tests that are common to confirm a preeclampsia diagnosis include:
Blood Tests
Blood tests can help your doctor measure how your kidneys and liver are functioning. They can also measure your white and red blood cell counts and platelet levels.
Urine Tests
Your doctor may collect a urine sample from you (sometimes more than one). This test measures the level of protein in your urine and uses a ratio of creatinine to protein. Creatinine is always present in urine.
Fetal Ultrasound
Even if you aren’t due for another ultrasound, your doctor will likely order one if they suspect you may have preeclampsia. A fetal ultrasound allows doctors to measure the baby’s size and weight, the amount of amniotic fluid and see how your baby is moving.
Nonstress Test
A nonstress test assesses how your baby moves and reacts. A biophysical profile test uses an ultrasound to measure the baby’s breathing, movement, muscle tone and the volume of amniotic fluid. During the process, the baby’s heart rate is consistently monitored.
Is There a Cure for Preeclampsia?
There is not currently a cure for preeclampsia aside from delivery. The best treatment is usually relegated to a lack of strenuous activity, often bed rest. For cases of mild preeclampsia, this may be all that is necessary to keep the pregnancy going until the baby is viable or full-term. Bed rest isn’t without risks, however, as it can increase the risk of blood clots. Medications, such as antihypertensives, corticosteroids, seizure prophylaxis during labor and anticonvulsants may also be necessary.
The goal of treatment is to keep the pregnancy healthy and the baby in the womb as long as possible. Sometimes bed rest is enough. But in more serious cases, the mother may require hospitalization until she delivers.
In severe cases of preeclampsia, doctors will most often schedule a Cesarean section (c-section). Mothers who are diagnosed towards the end of pregnancy, when the infant is viable, may have induced labor if a C-section is not necessary. This is so that the child stays as healthy as possible and doesn’t go into fetal distress. If doctors don’t manage labor carefully, the child can develop physical and neurological problems, and may have special needs well into childhood.
Unfortunately, because the only cure for preeclampsia is delivery, that often means women will need an emergency C-section and will delivery prematurely. This can further increase the risk of birth injuries. Infants born to mothers with this complication are at a higher risk of:
You should know that even after delivery and resolution of immediate preeclampsia symptoms, it can still take some time for your body to heal. If you have organ damage or seizures, the time it takes you to recover may be even longer. This can be frustrating when you are planning to take your new baby home, but it is important that you allow yourself time to heal.
Treating Preeclampsia
As noted above, there is no cure for preeclampsia and treatment generally consists of delivering the baby as soon as possible. In addition to delivering the baby, the mother may also need treatment for symptoms related to preeclampsia, such as seizures and high blood pressure. Doctors will also try to prevent preeclampsia from escalating to eclampsia or HELLP syndrome. The methods most commonly used to do so include:
Blood Pressure Medication
Blood pressure medications, called antihypertensives, lower your blood pressure when it is too high. There are many different types of antihypertensive medication, and your doctor should choose one that is safe for pregnancy and/or breastfeeding. You may need an antihypertensive if your blood pressure is consistently higher than 140/90.
Corticosteroids
Corticosteroids are useful in improving platelet levels and liver function in women with preeclampsia and HELLP syndrome. They are safe for use during pregnancy, and may be useful after pregnancy to improve function. During pregnancy, corticosteroids can help the baby’s lungs mature, which is helpful if your doctor thinks you will deliver early.
Anticonvulsant Medications
If preeclampsia is severe, you may need an anticonvulsant to prevent you from having seizures or a stroke. One of the most common treatments is magnesium sulfate. Doctors or nurses administer magnesium sulfate through an IV. Magnesium sulfate is a mineral that reduces the risk of having a seizure. It normally begins within 24 hours of delivering the baby, and may last for up to two days. There are some risks with using magnesium sulfate, such as magnesium toxicity, so your healthcare team will monitor you closely while you receive the medication.
These treatment options can help improve your symptoms and improve the prognosis for you and your baby. You should know, however, that fully recovering can take some time. Sometimes high blood pressure lingers for weeks or even months after birth. Unfortunately, some women experience long-term or lifelong health impacts.
How is Preeclampsia Related to Cerebral Palsy?
There is still much about cerebral palsy that doctors don’t quite understand. However, studies indicate that mothers who have preeclampsia are more likely to have children with cerebral palsy if the infant is born prematurely. In some cases, this complication causes mothers to go into labor early, delivering babies that are born at 37 weeks or earlier. Premature infants are more vulnerable to birth injuries and may have other medical problems that can lead to brain damage.
Doctors don’t quite know if preeclampsia causes cerebral palsy, but research suggests that mothers who deliver babies between the gestational ages of 32 and 36 weeks are almost five times more likely to have babies who develop cerebral palsy. This may be because of preeclampsia-associated conditions like brain damage or HIE, a condition that causes brain damage.
What Can I do to Prevent Preeclampsia?
Although there isn’t a cure yet, researchers continue to look for ways to prevent preeclampsia and related medical conditions. So far, research shows that some potentially successful prevention strategies include:
- Taking a daily low-dose aspirin
- Taking calcium supplements daily
- Restricting salt from your diet
- Increasing Vitamin D
It is generally a good idea to limit salt intake during pregnancy and to eat as healthy as possible. However, before taking any medications or vitamins, always consult your physician. Not every supplement or vitamin is appropriate for every patient or pregnancy.
Sadly, there is no way to predict who will get preeclampsia. That’s why it is so important for doctors to educate women about this risk during pregnancy. There are countless sorties of women who had it and didn’t know it who struggled with difficult pregnancies, emergency c-sections, loss of their child, and permanent damage. There are equally as many stories of families who suffered the sudden death of their pregnant loved one because of undiagnosed preeclampsia.
Can I Get Preeclampsia More than Once?
The short answer to this question is yes. The probability that you will get preeclampsia more than once depends on several things. According to the Preeclampsia Foundation, research shows that, if you had it in your first or a previous pregnancy, your chances of getting it again are around 20%. However, experts say that the risk is really anywhere from 5-80%. The risk depends on when you had it and how severe it was.
If you have or had preeclampsia and are planning to have more children, you should talk to your doctor about the risk. Many women are advised against subsequent pregnancies if they experienced organ damage or other medical problems that damaged their reproductive organs. Only your doctor can assess the risk and help you understand exactly what your risk factors are and what you can do to reduce the risk.
Sources:



