
Hydrocephalus
Hydrocephalus is a medical condition in which there is an unusual buildup of cerebrospinal fluid (CSF) in brain cavities known as ventricles. According to the National Institute of Nervous Disorders and Stroke (NINDS), the exact number of cases of hydrocephalus is hard to determine because it strikes both children and adults. Hydrocephalus can be a congenital condition. However, it can also be acquired in cases of head trauma before, during or after birth.
What is Hydrocephalus?
The condition’s name comes from the Greek words “hydro” (water) and “cephalus” (head). Its literal translation is “water on the brain,” but the liquid that accumulates in the ventricles is not water but cerebrospinal fluid (CSF). The word “encephalopathy” means damage to the brain. Therefore, sometimes hydrocephalus is referred to as hydro encephalopathy. The correct name for this condition, however, is hydrocephalus.
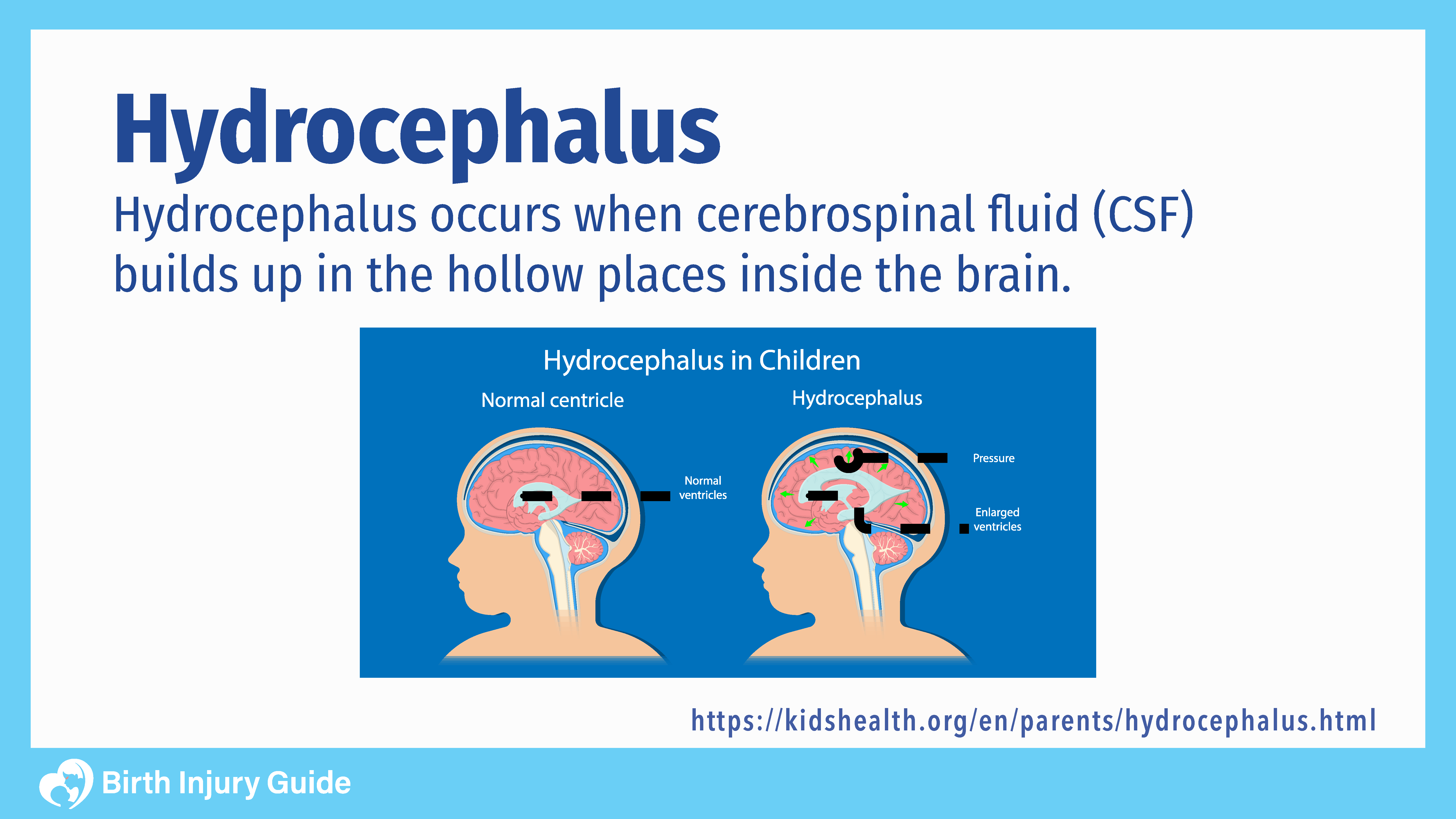
CSF is necessary for the brain to function. It protects the brain by serving as a cushion for the cerebral cortex. It also protects the brain from infections and minor impacts to the skull. Additionally, CSF helps regulate the involuntary function of the circulatory system in the brain.
CSF fits inside the subarachnoid space and within the ventricular system in and around the brain and the spinal cord. A healthy brain usually produces 500 milliliters (mL) of CSF daily. The central nervous system constantly reabsorbs CSF, so the average amount of the liquid within the brain and spinal cord at any time is approximately 100-160 mL.
Types of Hydrocephalus
Hydrocephalus’ various forms occur when there is a problem with the flow or reabsorption of CSF. According to NINDS, there are two main types of hydrocephalus: congenital and acquired:
- Congenital means it was present at birth.
- Acquired means that external factors, including other diseases or head trauma, usually cause the condition.
Both of the main forms of hydrocephalus come in two categories: communicating and non-communicating.
- Communicating: The ventricles of the brain are still open and CSF can still flow inside them. However, the CSF can’t flow out of the ventricles because the exits are somehow blocked.
- Non-communicating: The flow of CSF along the narrow passages that connect the ventricles is completely blocked. A common cause of non-communicative hydrocephalus is the narrowing of the passage called the aqueduct of Sylvius. This small pathway connects the third and fourth ventricles.
These forms of the condition mainly affect children. Per NINDs, the prevalence of hydrocephalus is around 1-2 per 1,000 babies born in the U.S.
What Causes Hydrocephalus?
In most cases, it is hard to identify what causes hydrocephalus. Genetic abnormalities or developmental disorders linked to conditions such as spina bifida sometimes cause the congenital forms of the condition. Other possible causes are meningitis, tumors, intraventricular bleeding or subarachnoid hemorrhages.
Traumatic head injuries before or during delivery can also cause blockages in the cranial ventricles and prevent the normal flow of CSF in a baby’s central nervous system.
Can Hydrocephalus be Prevented?
One of the primary conditions that often underlie hydrocephalus is an intracranial hemorrhage. Therefore, it is important to know the risk factors that may increase the chances of your child suffering an intracranial hemorrhage and/or hydrocephalus. By knowing these risks, you and your healthcare team can make every effort to prevent such injuries.
The primary risks of intracranial hemorrhage and/or hydrocephalus include:
- Premature birth
- Hypoxic ischemic encephalopathy (HIE)
- Infections
- Forceps delivery injury
- Vacuum extraction injury
Start Your FREE Case Review Today
If you or your child is injured as a result of medical negligence, call us to learn more.
Symptoms of Hydrocephalus
The severity of hydrocephalus symptoms depends on many variables, including a person’s age, how advanced the condition is and personal differences in tolerance for the disease. Some babies, for instance, don’t experience any negative effects from the condition because the size of their skulls increases. In these cases, CSF continues to flow normally among the ventricles because the elasticity of the still-growing skull prevents narrowing of the cranial passages.
In cases where the aqueduct of Sylvius and other passages are blocked, the symptoms are more severe. The most obvious signs of hydrocephalus in babies are an abnormally large head or an unusually fast increase of the head’s circumference. Parents may also note symptoms, such as:
- Headaches
- Irritability
- Vomiting
- Seizures
- Sleepiness
- Coma
Tests to Confirm Hydrocephalus Diagnosis
If your child’s doctor suspects that he or she has hydrocephalus, there are some head imaging tests that can confirm the diagnosis. These include ultrasounds, computed tomography (CT scan) and magnetic resonance imaging (MRI). These tests can show the presence of enlarged ventricles or an increase in intracranial pressure. Head imaging tests can also distinguish between the different types of the condition, which is important in determining treatment options.
Treatment for Hydrocephalus
Shunt surgery is the most common method of treating hydrocephalus. Doctors generally insert catheters, called shunts, into the cerebral ventricles. The shunts allow CSF to flow normally in the central nervous system and prevent further accumulation of the liquid in the ventricles. The excess fluid flows into other spaces in the body and is then reabsorbed.
Another surgical treatment for hydrocephalus is a procedure called third ventriculostomy. Using a tiny fiber optic camera called a neuroendoscope, doctors inspect the ventricular surface. When the neuroendoscope is in place, they use a tiny tool to drill a small opening on the third ventricle’s floor. This hole removes the blockage in the ventricle and allows the CSF to flow normally again.
Both forms of treatment usually work well, but there can be complications if problems occur with shunts. The two main problems associated with surgically-implanted shunts are:
Shunt failures
According to the Hydrocephalus Association, 50 percent of all shunts fail within two years. They usually fail due to the natural changes in the skull as a child gets older. Shunts are made to last a long time and are resilient, but the components can wear out over time. In some cases, they can get loose or break in several pieces.
Shunts can also be clogged or get disconnected. Shunt failure results in renewed pooling of CSF and the return of symptoms. Per the Mayo Clinic, additional symptoms of shunt failure in infants includes:
- Fever
- Irritability
- Sleepiness
- Poor feeding
- Vision problems
Shunt systems need both constant monitoring and regular medical follow-ups. This helps to keep the negative effects of shunt failure under control and allows physicians to schedule shunt replacement operations to prevent further complications.
Shunt Infections
Per the Hydrocephalus Clinical Research Network (HCRN), an estimated 6-10 percent of shunt procedures result in infections. Bacteria already present on the skin of the child often cause shunt infections. Symptoms may include redness or tenderness along the shunt tract, sore neck or shoulder muscles and a low-grade fever.
Prognosis
According to Boston Children’s Hospital, the long-term outlook for a child with hydrocephalus depends on early detection, timely treatment of the condition and preventing infection during surgery. Shunts and third ventriculostomies relieve the pressure inside the skull and prevent more neurological damage. Nevertheless, some children may still experience adverse effects such as persistent headache even though the intracranial pressure is gone.
Because medical researchers don’t have a clear understanding about hydrocephalus, there is no easy way to predict general outcomes. Medical researchers know that there is a connection between specific causes of hydrocephalus and their outcomes. Beyond that, predicting a specific child’s prognosis depends on such variables as early detection of the condition, if any other disorders are present and how well the child responds to treatment.
Because hydrocephalus often causes neurological damage, it can have a negative effect on a child’s intellectual and physical development. If left untreated, progressive hydrocephalus can be fatal.
How to Optimize Your Child’s Prognosis
Parents and loved ones should know that a hydrocephalus diagnosis is not necessarily a death sentence for a baby. Effective treatments for this condition do exist and are often successful. Proper monitoring by parents and caregivers can minimize its effects. As a result, many children with hydrocephalus grow up to lead normal lives with relatively few difficulties.
Sources:
- http://www.ninds.nih.gov/disorders/hydrocephalus/detail_hydrocephalus.htm
- http://www.hydroassoc.org/?s=+Hydrocephalus+education+and+support
- http://www.childrenshospital.org/health-topics/conditions/hydrocephalus
- http://www.mayoclinic.org/diseases-conditions/hydrocephalus/basics/definition/con-20030706
- http://www.hcrn.org/



