Chorioamnionitis
Chorioamnionitis is an inflammation of the fetal membranes due to a bacterial infection. It is often caught in the mother’s urogenital tract and works its way up towards the baby, infecting the fetal membranes, and causing a number of problems for both mother and baby.
If left untreated, the mother may develop pelvic or uterine infections, endometriosis, blood clots and/or sepsis.
What is Chorioamnionitis?
As noted above, chorioamnionitis is a bacterial infection that develops before or during labor. The name comes from “chorion”, or the outer membrane, and “amnion”, or the fluid-filled sac. When bacteria develops in the chorion, amnion, and/or the amniotic fluid around the baby, it can cause problems with the pregnancy, labor and delivery.
Most often, chorioamnionitis occurs in premature infants. It is estimated that only two to four percent of full-term births will involve the condition.
What Causes Chorioamnionitis?
Maternal infection is the primary reason for developing chorioamnionitis, and it usually develops in the mother’s vaginal area. The bacteria that causes this kind of serious maternal infection includes anaerobic bacteria, E. coli and group B streptococci. The mother should report any symptoms of a bacterial infection immediately.
Furthermore, doctors should treat these symptoms of infection as serious so that chorioamnionitis doesn’t develop.
Can Chorioamnionitis be Prevented?
The best way to prevent chorioamnionitis is to understand the risk factors and make sure you discuss them with your doctor prior to labor and delivery. Risk factors include:
- Young maternal age, generally less than 21 years old
- First pregnancy
- Prolonged rupture of membranes (> 18 hours)
- A long, stressful labor
- Premature labor
- Pre-existing infections
What are the Symptoms of Chorioamnionitis?
Because this particular condition affects an infant while still in utero, it is the mother that experiences the symptoms of chorioamnionitis. The most common symptoms are:
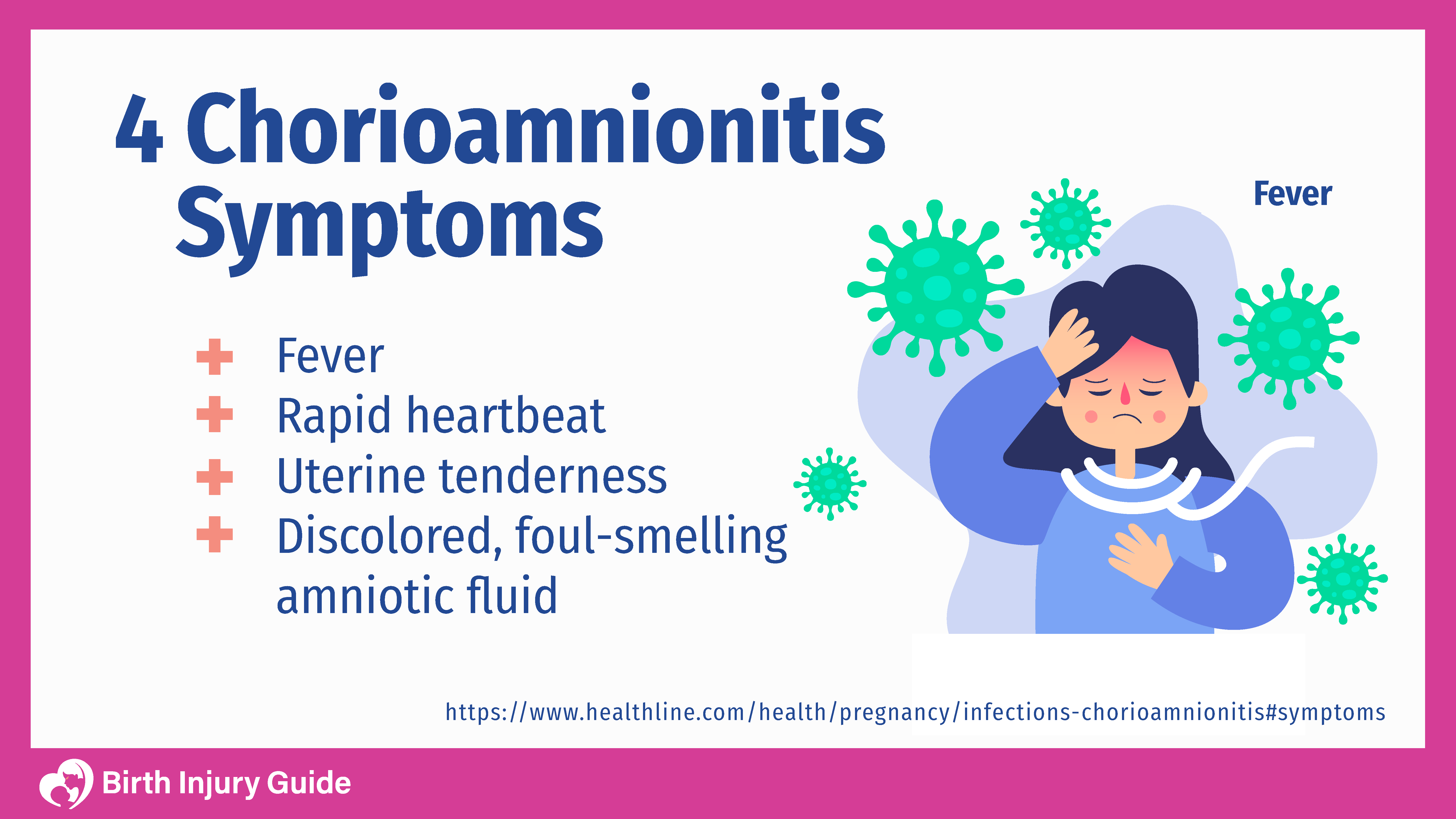
Other symptoms may include:
- Fetal tachycardia
- Maternal leukocytosis
- Vaginal discharge
For infants, a diagnosis of neonatal sepsis is generally made based upon the following symptoms:
- Weak cries, poor sucking and fatigue
- Pulmonary problems, such as respiratory distress, apnea, and cyanosis
- Gastrointestinal problems, which may include bloody stools, vomiting and diarrhea
- Seizures
- Hematologic problems, such as pallor or purpura
How Chorioamnionitis Affects Children
Chorioamnionitis can be serious. Infants may develop sepsis as a result of the infection, which can be extremely dangerous. A diagnosis of neonatal sepsis is generally made based upon the following symptoms:
- Weak cries, poor sucking and fatigue
- Pulmonary problems, such as respiratory distress, apnea, and cyanosis
- Gastrointestinal problems, which may include bloody stools, vomiting and diarrhea
- Seizures
- Hematologic problems, such as pallor or purpura
It is important to accurately diagnose chorioamnionitis or neonatal sepsis immediately in order to avoid possible complications.
Tests to Confirm a Diagnosis of Chorioamnionitis
Sometimes there are few or no outward symptoms in the mother. For this reason physicians generally diagnose chorioamnionitis by checking for an increased heart rate in both mom and baby. However, according to the National Institutes of Health (NIH), maternal fever is one of the most prominent indications of chorioamnionitis. Mothers typically have a recurring fever of over 100 F, which is considered abnormal during pregnancy.
If that happens, your doctor may order an amniocentesis test, which takes a small amount of amniotic fluid from the womb for testing. If the amniotic fluid has low concentrations of glucose and high concentrations of white blood cells or bacteria, you may have chorioamnionitis.
During pregnancy, laboratory tests may be performed in order to check the mother’s blood and urine, and to rule out group B strep infection. In addition, the amniotic fluid is examined for abnormalities, bacterial culture, glucose concentration, gram staining and pH levels.
Mothers may also be tested for:
- White blood cell counts
- Levels of C-reactive proteins
- Alpha1-protein measurement
- Ferritin levels
Treatment for Chorioamnionitis
Because chorioamnionitis is so dangerous, the treatment for the infant is generally a hasty delivery. In most cases, the mother is given antibiotics, and if needed, the infant may be prescribed antibiotics as well.
Other forms of treatment may include:
- Infant intubation and ventilation
- Balancing glucose levels
- Artificial breathing tubes for the infant
Prognosis for Chorioamnionitis
If an infection or chorioamnionitis is caught immediately and the infant is given antibiotics, the infant will usually not have any long-term effects due to chorioamnionitis. However, if the infection is not immediately caught, the child’s side-effects could include:
- Sepsis
- Meningitis
- Severe respiratory problems
- Pneumonia
- Brain damage
Infants who are born prematurely are at a heightened risk for developing these medical conditions, but the risk is still relatively rare. There is, on average, a 10-20 percent chance of developing pneumonia and a 15 percent chance of developing brain complications.
How to Optimize Your Child’s Prognosis
The prognosis for mothers who develop chorioamnionitis is very good. The only real long-term impact is possible fertility problems. For infants, the prognosis is also generally favorable. Some infants may have long-term complications, but that generally only occurs in the most severe cases, such as those that develop into sepsis or meningitis.
As a parent, the best thing you can do to optimize your child’s prognosis is to work closely with a healthcare team who can address any short- and long-term impacts.
Start Your FREE Case Review Today
If you or your child is injured as a result of medical negligence, call us to learn more.