
Neonatal Sepsis
Neonatal sepsis is a potentially life-threatening bloodstream infection that affects newborns. Sepsis is a serious medical condition that can cause serious injuries like brain damage, and can cause life-altering complications or even death.
It is imperative that healthcare providers understand the risks of neonatal sepsis and take measures to prevent it. That includes identifying maternal infections and taking measures to prevent the infection from spreading.
If a newborn does develop sepsis, immediate treatment is the only way to reduce the risk of serious injury or death.
The mortality rate among infants with untreated sepsis is around 50%.
What Causes Neonatal Sepsis?
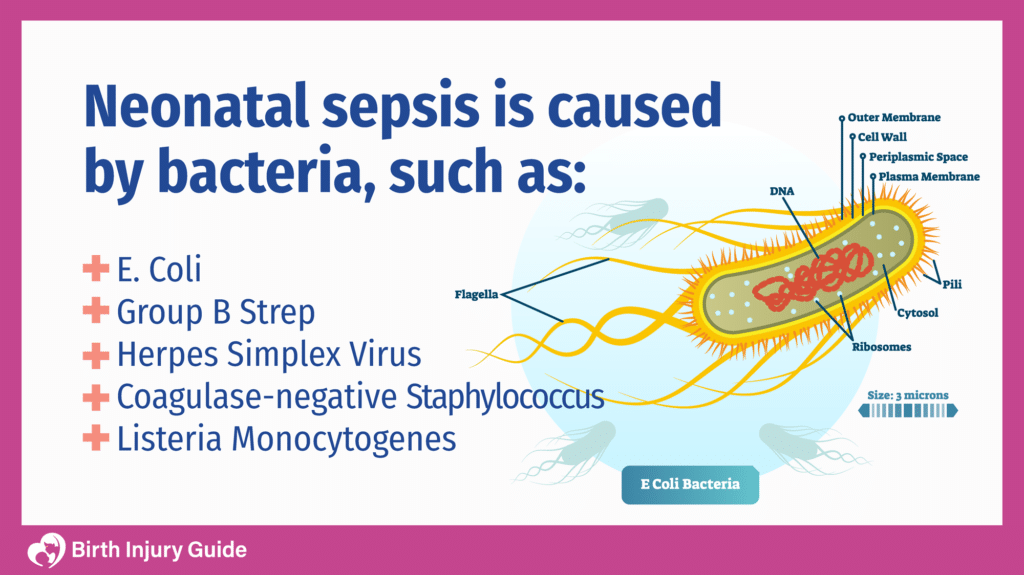
Neonatal sepsis can be caused by a variety of bacteria, viruses and pathogens. Infants can get sepsis by either vertical or horizontal transmission:
- Vertical Transmission: A maternal infection spreads to the baby shortly before delivery, or during delivery.
- Horizontal Transmission: The baby acquires an infection due to contact with environmental contaminants, caregivers or healthcare providers.
One of the best ways to prevent transmission is for healthcare providers to recognize maternal infections and treat both mother and child as necessary.
Bacteria and viruses can live in the mother’s genitourinary tract, including the cervix. During labor and delivery, microorganisms can be transmitted to the infant as it passes through the birth canal.
In addition to maternal infections, there are also some risk factors that expectant parents and healthcare providers should be aware of. Risk factors for neonatal sepsis include:
- Premature rupture of the membranes (water breaking)
- Premature birth
- Chorioamnionitis
- Poor prenatal care
- Birth asphyxia
- Meconium staining
- Urinary catheterization
- Mechanical ventilation
- Poor feeding advancement
Infants who are born prematurely or who have a low birth weight are more at risk for infections and sepsis. The risk of sepsis, and the risk of sepsis-related death, is much higher among premature infants than full-term infants.
Symptoms of Neonatal Sepsis
It is important that healthcare providers and parents know the risk factors and symptoms of sepsis. If symptoms appear, parents should alert their healthcare provider immediately. Newborns with neonatal sepsis may exhibit some or all of the following symptoms:
- Breathing problems
- Changes in body temperature
- Diarrhea
- Low blood sugar
- Reduced movement
- Reduced sucking/feeding
- Seizures
- Abnormal heart rate
- Abdominal swelling
- Jaundice
Diagnosis and Treatment
The symptoms of neonatal sepsis are considered “nonspecific”. That means that the symptoms most often experienced are also possible symptoms of other conditions. Diagnosis and treatment are imperative to preserving the health of the infant and improving the prognosis.
Diagnosing Neonatal Sepsis
Diagnosing neonatal sepsis requires a thorough physical examination and assessment of symptoms and other factors.
Healthcare providers will also order lab tests that will help identify sepsis or other medical conditions. Lab tests that can help diagnose sepsis include:
- Complete blood count (CBC)
- C-reactive protein
- Blood culture
Sometimes, doctors will order a spinal tap. This process involves inserting a long needle into the spinal area. Fluid is withdrawn and then examined for the presence of bacteria.
Other tests that can confirm a sepsis diagnosis and check for complications include x-rays, urine cultures and skin tests.
Neonatal Sepsis Treatment
The primary method of treating neonatal sepsis is antibiotics. The type and course of antibiotics will depend on the child’s age and other factors. A general idea of how antibiotic treatment may occur includes:
- Infants younger than four weeks old who have signs of infection and/or a fever will receive antibiotics (IV) immediately.
- If the mother had chorioamnionitis or other risk factors, the infant will receive IV antibiotics, even if there are no symptoms present.
- If bacteria is found in the spinal fluid, the infant will receive antibiotic treatment for up to three weeks.
- For infections related to the herpes simplex virus (HSV), infants may receive acyclovir, an antiviral medication.
Ultimately, the method and duration of treatment will depend on your child’s health and the underlying cause of sepsis. It is important to discuss treatment options with your child’s doctor, and understand any possible risks associated with certain treatments.
Prognosis for Neonatal Sepsis
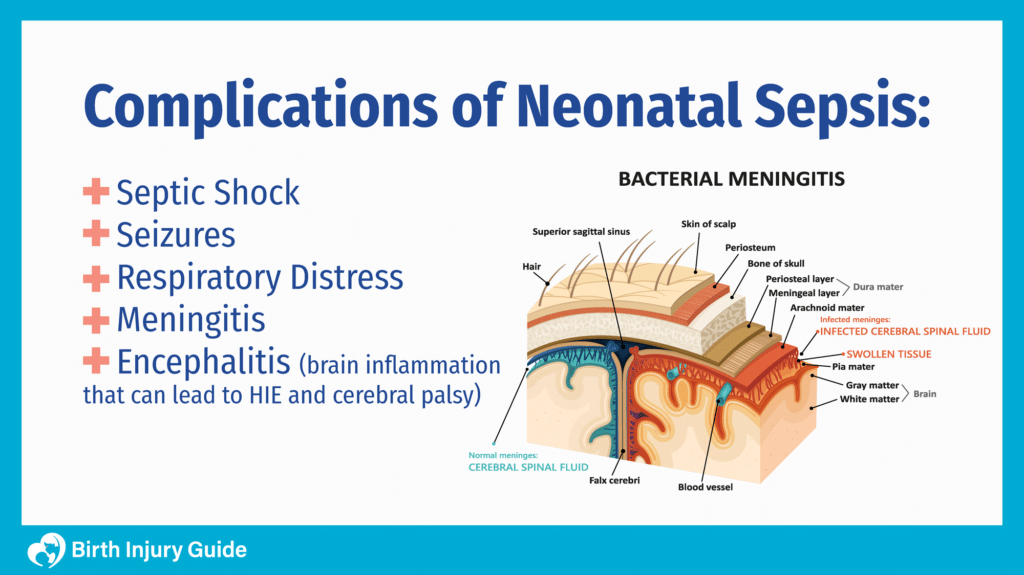
Early diagnosis and treatment are crucial for a positive outcome. Generally, infants who receive immediate diagnosis treatment will recover without long-term health problems. If, however, risk factors and symptoms are missed, diagnosis and treatment may be delayed. This increases the risk of complications or death.
For infants who have sepsis and survive, there is a risk of long-term health conditions, including cerebral palsy, vision impairment, developmental delays and other neurodevelopmental disabilities.
If the infant has meningitis, he or she is also at risk for hydrocephalus and periventricular leukomalacia.
Neonatal Sepsis as a Birth Injury
A birth injury is any harm that happens to an infant during the labor and delivery process, and in the period of time just after birth. Neonatal sepsis can be a birth injury if healthcare providers fail to take preventative measures, fail to treat sepsis in a timely manner or otherwise fail to adhere to the standards of care when treating the infant.

If you believe your child has suffered a birth injury, contact Birth Injury Guide to learn more about your legal rights. Healthcare providers must be held accountable when their negligence causes harm to a patient. As a parent, you may be able to take action on your child’s behalf.
Start Your FREE Case Review Today
If you or your child is injured as a result of medical negligence, call us to learn more.
Sources:
- https://medlineplus.gov/ency/article/007303.htm
- https://emedicine.medscape.com/article/978352-clinical#b3
- https://www.merckmanuals.com/professional/pediatrics/infections-in-neonates/neonatal-sepsis
- https://jamanetwork.com/journals/jamapediatrics/article-abstract/2765163
- https://pediatrics.aappublications.org/content/129/5/1006
- https://medlineplus.gov/ency/article/007303.htm
- https://emedicine.medscape.com/article/978352-clinical#b3
- https://www.merckmanuals.com/professional/pediatrics/infections-in-neonates/neonatal-sepsis
- https://jamanetwork.com/journals/jamapediatrics/article-abstract/2765163
- https://pediatrics.aappublications.org/content/129/5/1006
- https://neonatalsepsiscalculator.kaiserpermanente.org/



