
Umbilical Cord Compression
During pregnancy, the umbilical cord is the baby’s lifeline. It is what provides the baby with oxygen, blood and vital nutrients throughout the pregnancy and into labor and delivery. The umbilical cord is, essentially, what the baby eats and breathes through, and it transports waste back to the placenta from the baby. If something goes wrong with the umbilical cord, the baby’s health is put at risk. One major complication involving the umbilical cord is umbilical cord compression.
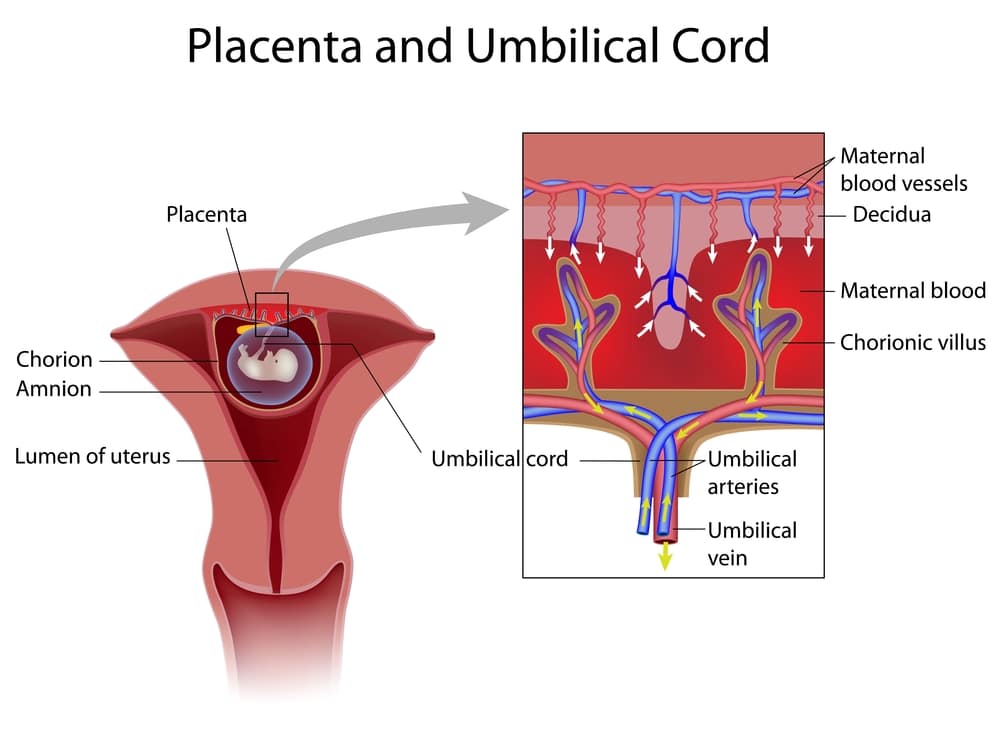
Umbilical cord compression occurs when a baby’s umbilical cord becomes flattened by pressure. A flattened, or compressed, cord can restrict blood flow and oxygen to the baby. This causes heightened and extremely dangerous health risks for the infant. Although it’s an easy condition to recognize, immediate treatment is extremely important.
What Causes Umbilical Cord Compression?
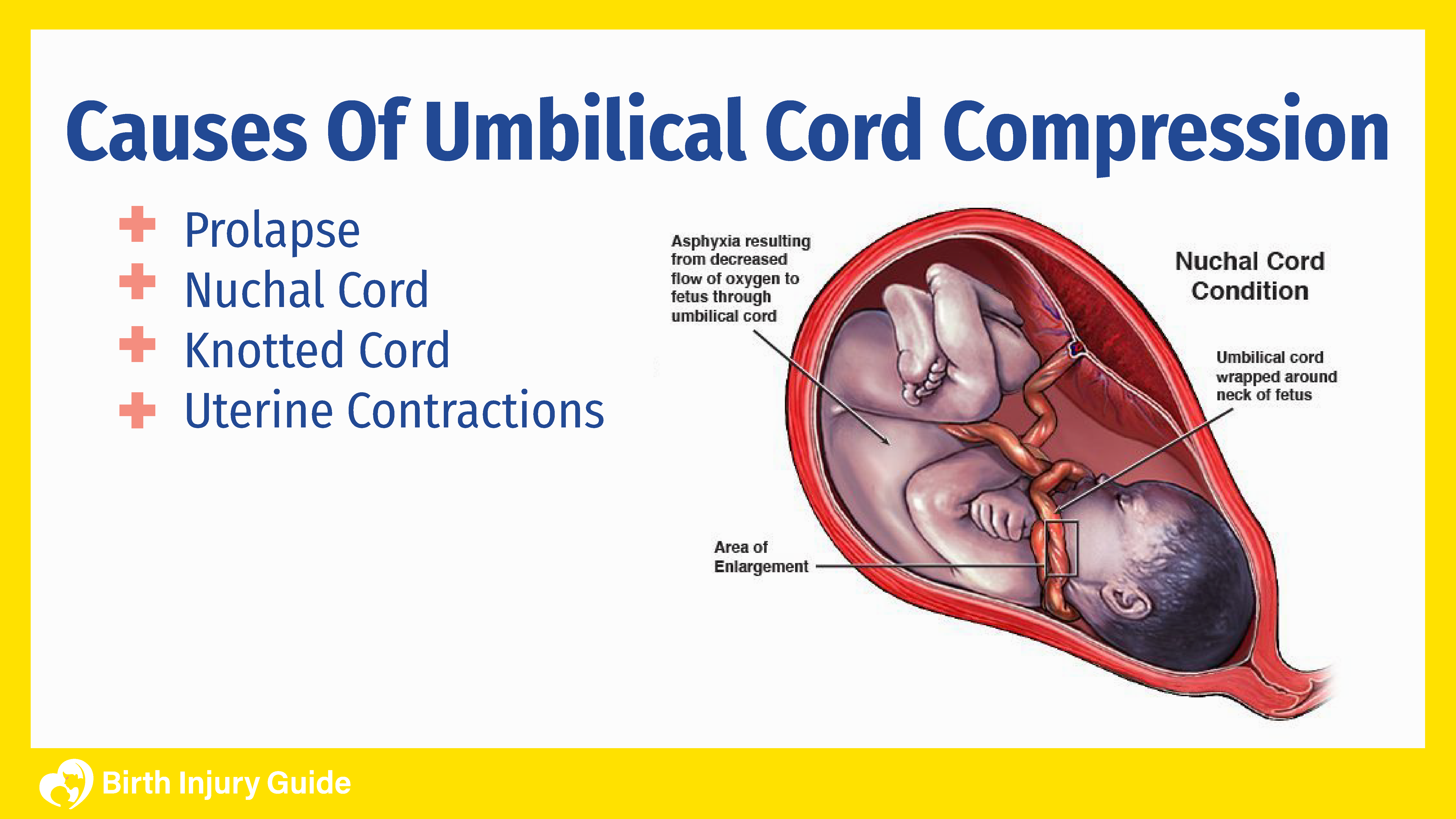
Umbilical cord compression can be caused by anything that results in the cord becoming compressed. The most common cause is the baby squeezing or lying on the cord in the uterus. It can also be squeezed by excessive uterine tone. The most common causes of compression are prolapse, nuchal cord, knotted cord or uterine contractions.
Umbilical Cord Prolapse
Typically, when a baby is delivered vaginally, the baby’s head comes out first, followed by the body, then the umbilical cord. An umbilical cord prolapse occurs when the cord moves into the birth canal ahead of the baby or at the same time. This causes the cord to be compressed between the baby and the birth canal or cervix. A cord prolapse is more common among women whose membranes rupture (water breaking) before labor begins.
Nuchal Cord
A nuchal cord is the medical term for what happens when the umbilical cord gets wrapped around the baby’s neck. Sometimes, the cord wraps just once, and other times it can wrap numerous times. Nuchal cord is fairly common, and doctors generally know how to handle these situations quickly and safely. Unfortunately, a nuchal cord can cause oxygen deprivation and a lack of blood flow to the baby, which can be dangerous.
Knotted Cord
A knotted umbilical cord, or “true knot”, occurs when the umbilical cord gets tied in a knot. If the knot is tight enough, the cord may become compressed. Knotted cords are more common during early pregnancy when the fetus is smaller and moves around a lot. It is also more common in women who are an “advanced maternal age” and who have had previous pregnancies.
Uterine Contractions
Some degree of umbilical cord compression is natural during uterine contractions. When this happens, however, compression is temporary and periodic. It becomes a medical emergency if the compression is longer-lasting or does not seem related to contractions.
Low Levels of Amniotic Fluid
Low levels of amniotic fluid is a medical condition called oligohydramnios. Amniotic fluid is important to protect the growing fetus, providing cushioning and helping the baby grow. If there is a low level of amniotic fluid, there is a greater chance of umbilical cord problems, including compression.
Risk Factors for Umbilical Cord Compression
Umbilical cord compression is often an unpredictable part of pregnancy, labor or delivery. However, there are some risk factors that may increase the risk of it occurring. Parents and healthcare providers should be aware of these risks and be diligent in monitoring the mother and baby.
Risk factors for cord compression include:
- A breech delivery
- Premature delivery
- Carrying twins
- Unusually long umbilical cord
Umbilical Cord Compression Injuries
Any sort of change, injury or trauma to an infant’s umbilical cord can result in serious medical issues. If an umbilical cord becomes compressed oxygen, blood flow, and nutrients can be cut off from the baby. This can result in umbilical cord compression injuries like brain damage and, in severe cases, fetal death. Fortunately, umbilical cord compression can be detected easily and if treated quickly, the aforementioned medical problems may be eliminated. However, when an infant lacks oxygen, every second is crucial. It’s imperative that physicians act fast once umbilical cord compression is recognized.
Umbilical cord compression can affect the baby’s health – immediately after birth and potentially into their childhood and beyond. Some of the possible medical conditions that baby’s may suffer include:
- Brain damage
- Fetal heart abnormalities
- Poor physical development
- Birth injuries associated with emergency cesarean sections (C-sections) such as fetal lacerations, bruising, and sometimes swelling
Any of these medical risks can have a profound impact on your baby and family. Talk to your doctor about possible umbilical cord issues and your risk level. Suspected umbilical cord compression should be taken very seriously by your healthcare team.
Brain Damage and Cerebral Palsy
If umbilical cord compression causes brain damage, the baby is at risk for cerebral palsy. Cerebral palsy is a series of motor disorders that affect movement, balance, posture and motor control. Every year, between 8,000 and 10,000 people are diagnosed with some form of cerebral palsy – spastic, athetoid, ataxic or mixed varieties. Depending on the type of cerebral palsy the child has, they may have symptoms like abnormal movements, floppy muscle tone, stiff muscles, paralysis or missed developmental milestones.
Cerebral palsy is a disorder for which there is no cure. It is a lifelong disorder that will impact the child and family forever. There are treatments available that can help manage the symptoms of cerebral palsy, particularly pain, speech, movement, behavioral issues and motor skills. Physical therapy is one of the most highly recommended treatment options, along with certain medications that can help manage pain and muscle spasms.
Because cerebral palsy is a disorder that affects everyone just a bit differently, the treatment options for your child may not be the same as other children – even if their conditions are similar. The best course of action if your child has cerebral palsy is to develop a care plan involving doctors, therapists and specialists from various medical disciplines. This comprehensive approach to treatment ensures that your child has the best chances for a quality, fulfilling life.
Signs of Umbilical Cord Compression
Sometimes, umbilical cord compression is not immediately recognizable. This is especially the case when the baby is still in the womb. The good news, however, is that routine prenatal care and ultrasounds can help identify the signs of umbilical cord compression or other similar complications. Some of the things that doctors look for include:
Heart Rate Changes
A change in an infant’s heart rate is one of the first recognizable symptoms of umbilical cord compression. The baby’s heart rate may decelerate quickly, therefore it’s imperative that fetal monitoring is being adhered to. Usually, it quickly returns to a normal rate. The heartbeat typically declines to less than 100 beats per minute (BPM).
Umbilical Cord Drop
Sometimes, when the umbilical cord begins to prolapse, the mother can feel it dropping into the birth canal when her water breaks. For pregnant mothers, it is important to convey any such feeling to your doctor right away.
Reduced Fetal Movement
In addition, pregnant women may be able to tell a difference in movement shortly after an umbilical cord compression. The baby’s movements may become a lot less frequent. Furthermore, when the amniotic sac ruptures, the mother may be able to physically feel the cord dropping into the birth canal if it prolapses.
Intrauterine Growth Restriction (IUGR)
During prenatal care, your doctor will routinely measure the baby via ultrasound. This tells the doctor whether the baby is growing at a normal rate for the pregnancy. If the umbilical cord is compressed, the baby may not be getting adequate nutrition, which can cause them to be growth restricted. If that is the case, you may not know that the cord is compressed until the baby is diagnosed with IUGR.
Treating Umbilical Cord Compression
Treatment of umbilical cord compression is based on the underlying cause of the compression, as well as how severe the compression is. Doctors will also factor in the health of the mother and baby, and how likely it is that the compression will cause problems as pregnancy continues.
Treating Minor Compression
For minor umbilical cord compression, sometimes changing the mother’s position change is all that is needed to relieve the compression. Amnioinfusion is another treatment option that can help minor or moderate compression. Amnioinfusion is the process of adding saline solution to the womb in order to relieve pressure that may be causing cord compression.
Treating Moderate Compression
In more moderate cases, additional oxygen and fluids are given to the mother in an attempt to push more oxygen and nutrients through the placenta to the infant. As labor progresses, doctors may use medications to try to stop contractions long enough for the baby to recover and for the compression to resolve.
Treating Severe Compression
In many cases, the umbilical cord either moves away from the birth canal or becomes uncompressed in time before the infant becomes too distressed. During delivery, the doctor may be able to slide their fingers under the umbilical cord and move it so that it is not compressed. Once a mother’s water breaks, however, if there is a rapid decrease in fetal heart rate, then physicians must treat the situation as an emergency and act accordingly. For severe cases of umbilical cord compression or prolapse, an emergency c-section may be necessary, and is often carried out as soon as fetal distress is detected.
Prognosis for Infants
The outlook after an umbilical cord compression is generally good as long as the healthcare provider detects and treats the problem in a timely manner. As mentioned earlier however, failure to recognize the signs of umbilical cord compression and treat it fast enough can lead to lack of nutrients, oxygen, and blood flow to the baby. This in turn, can lead to severe brain damage, causing cerebral palsy (CP), autism, behavioral disorders, and fetal death.
Start Your FREE Case Review Today
If you or your child is injured as a result of medical negligence, call us to learn more.



