
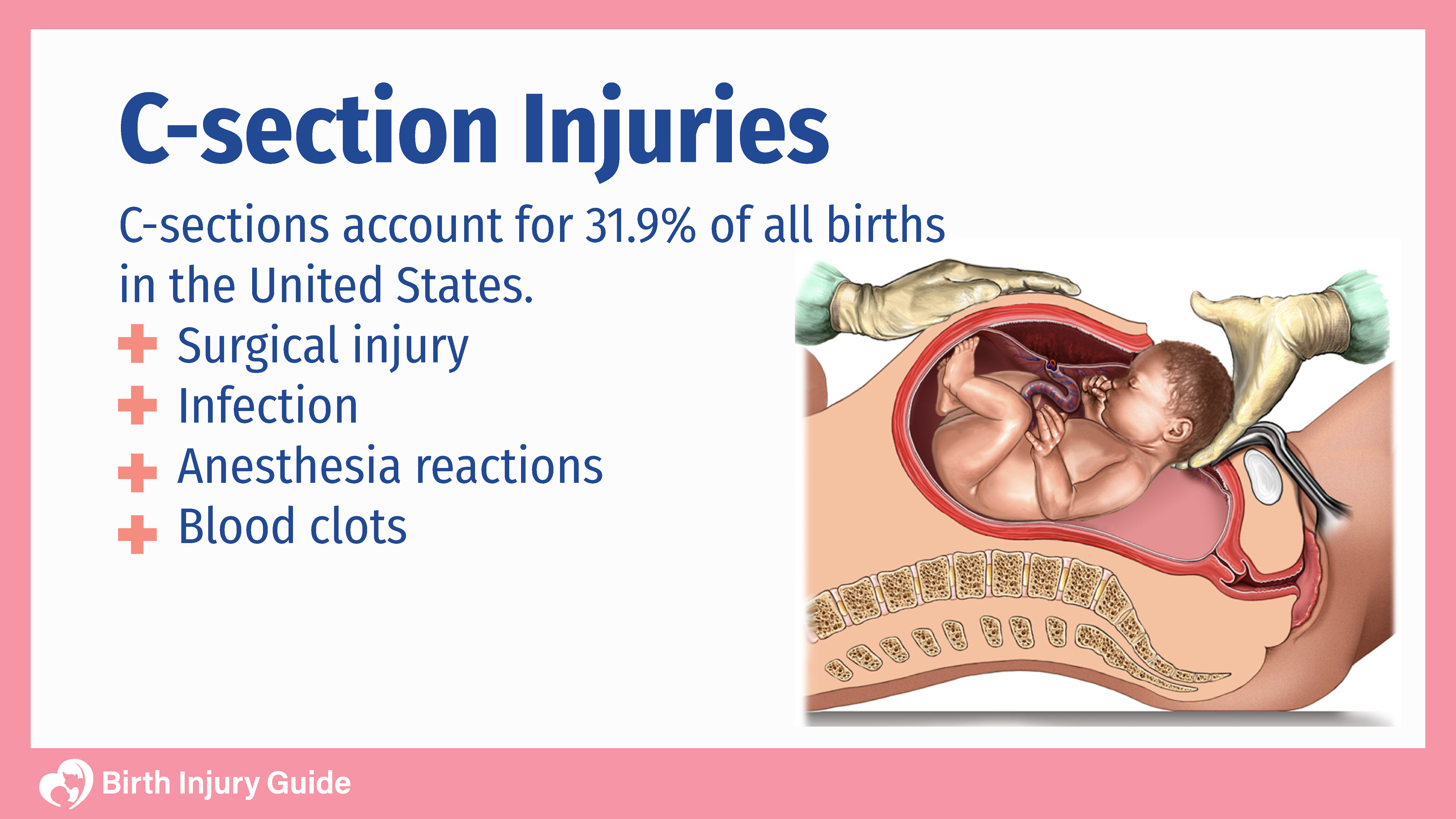
C-Section Injuries
During labor and delivery, there are two incredibly important things that healthcare providers must do. First, they must recognize signs of fetal distress or complications that may cause fetal distress. Next, they must be willing and able to perform a cesarean delivery (c-section) in the event of a complication or medical emergency. These are two of the best ways that healthcare providers can reduce the risk of birth injuries when a vaginal delivery is not optimal. During this process, healthcare providers must also do what they can to reduce the risk of c-section injuries.
There are various types of c-section injuries that can affect the health of the mother and baby. Not only are there risks to c-sections (as with any surgery), but there are also risks to the baby’s health if a c-section is not performed in a timely manner when it is necessary. Failure to recognize fetal distress or order a c-section when necessary is medical negligence. In these cases, it is important that parents understand their rights and the situation that they now find themselves in.
Below, the team at Birth Injury Guide explores c-sections, possible injuries, and the birth injuries that can occur and impact your family. As always, if you have questions, please don’t hesitate to reach out to our birth injury lawyers.
Start Your FREE Case Review Today
If you or your child is injured as a result of medical negligence, call us to learn more.
What is a Cesarean Section (C-Section)?
Cesarean delivery, or C-section, is a surgical procedure that delivers a baby through incisions in the abdomen rather than a vaginal delivery. The surgeon makes incisions in the abdomen and through the uterus to deliver the baby. During a C-section, you are awake. Before the procedure begins, an epidural or spinal block is injected into the lower back. This makes you numb from the chest down. After that, you will have a urine catheter inserted and will be cleaned and sterilized. The operating room team will place curtains near your chest so you can’t see what is happening, but you are awake and can communicate with your partner and healthcare team.
After the baby is delivered, you will be able to immediately see and cuddle him or her. Unless there are medical reasons why you can’t, you may even be able to immediately breastfeed. Once you are sutured and cleaned up, you and your baby will move to a recovery area.
Common Reasons Doctors Perform C-Sections
Cesarean sections (C-sections) have increased in popularity over the past few decades. In 2010 alone, a little over 32 percent of all deliveries in the United States were C-sections. There are a myriad of reasons why C-sections are performed. Most often, they are performed out of medical necessity. In some cases, c-sections are planned if it is less risky to the mother or baby than a vaginal delivery. While the reason may vary, one thing each C-section has in common is that there is a risk of C-Section injuries to both mother and infant.
There are several reasons why a physician may feel a C-section is necessary or in the best interests of safety. Some of the most common reasons include:
- Placental problems, including placental abruption (premature separation of placenta), placental insufficiency and placenta previa
- Uterine ruptures, which affects 1 out of every 1,500 births
- An infant in the breech position, making normal delivery difficult
- Umbilical cord prolapse
- Fetal distress
- No progress during labor and attempted vaginal birth
- Having previous C-sections
- Preeclampsia
- Diabetes
- Genital herpes (active)
- An infant diagnosed with a birth defect
- Carrying twins or multiples
What are C-Section Injuries?
Unfortunately, there are still risks involved with C-section deliveries. While some injuries cannot be predicted or prevented, others are a direct result of medical errors or medical negligence.
Some of the most common c-section injuries affecting mothers include:
Anesthesia Injuries
During a C-section, the mother is administered medications to ensure pain relief, usually an epidural or spinal block. It is extremely important that the dosage is not only correct but that the mother isn’t allergic to it. Incorrect dosage or complications can lead to anesthesia injuries, such as:
- Extremely low blood pressure
- Internal bleeding
- Blood clots
- Severe headaches
- Placenta previa
- Placental abruption
Maternal Surgical Injuries
Maternal surgical injuries are extremely rare, but if they occur, life-threatening health issues may follow. Surgical injuries happen when a nearby organ is cut or affected in some way during the C-section. If organs like the bladder or intestines are cut, additional surgery may be required to repair the damage.
Maternal Infections
Maternal infections are a possibility after any type of surgery, including C-sections. Physicians must be extremely careful to ensure proper sterilization of the incision site. They must also provide proper post-surgery treatment, such as antibiotics and appropriate wound care. When the mother does not receive appropriate care, she is at risk for infections, such as:
- Streptococcus
- Endometritis
- Intra-amniotic infection, which increases the risk of a postpartum infection
- Extremely high fever
If a mother has an infection already, it can be transmitted to the baby if the doctor attempts a vaginal delivery as well. It is important to assess infection risk during vaginal birth as well as during surgery.
Blood Clots
Blood clots are another risk after a C-section. However, they can be prevented in many cases if the mother is monitored and allowed to walk within 24 hours after the surgery. If a blood clot develops, there is a risk that it will break apart and travel to other parts of the body, including the brain, heart and lungs.
Hemorrhaging
There is always a chance of increased bleeding after a surgical procedure. After a C-section, if bleeding is not kept under control, hemorrhaging may occur. Severe hemorrhages or uncontrolled bleeding may require a blood transfusion.
Birth Injuries Caused by C-Section Injuries
In addition to the injuries that a mother may experience during a c-section, there are also birth injuries that can result from c-section injuries, including a doctor’s failure to perform a c-section, failure to perform one in a timely manner or making a mistake during the procedure. In some instances, physicians fail to schedule a C-section despite the fact that warning signs are present. For example, fetal distress is one of the most common reasons that C-sections are ordered. A delayed C-section can be caused by failure to closely monitor the mother or infant for signs of distress.
A delayed C-section can lead to a myriad of injuries. In the most severe cases, infant death may occur.
Some of the possible birth injuries include:
Infant Brain Damage
One of the most common types of fetal distress is oxygen deprivation. During pregnancy, labor or delivery, if the baby is deprived of oxygen, they can experience a variety of birth injuries, including brain damage. Brain damage is a birth injury that can cause a host of problems for the infant, including cognitive symptoms, developmental delays, physical symptoms and disorders like cerebral palsy.
Hypoxic Ischemic Encephalopathy
Hypoxic ischemic encephalopathy, or HIE, is a type of brain damage caused by a lack of oxygen during labor and delivery. There are several situations that can lead to HIE, including prolonged labor, placental issues, umbilical cord issues or infections. All of these factors can lead to oxygen deprivation and, consequently, HIE.
Cerebral Palsy
Oxygen deprivation, brain injuries and HIE can all lead to a baby developing cerebral palsy. Sadly, thousands of cases of cerebral palsy diagnosed each year are due to medical errors, including:
- Failure to properly monitor maternal and fetal vital signs
- Failure to order a timely c-section
- Inappropriate use of forceps or vacuum extraction
- Failure to diagnose or treat infections
- Failure to correct umbilical cord issues
Cerebral palsy is a disorder that will affect the child for their entire life. There is no cure – only treatment options that can help manage symptoms and improve overall quality of life. It is important to note that some types of brain damage that cause cerebral palsy can occur during a vaginal birth, as well as during a c-section.
Fetal Lacerations
Fetal lacerations are cuts, scrapes and other similar injuries to an infant that can occur during a C-section procedure. In most cases, fetal lacerations occur due to a surgeon improperly making incisions or scraping the baby with surgical tools during delivery. Fetal lacerations range in severity, from mild to serious, and may lead to a host of other health conditions, including Erb’s palsy, Klumpke’s palsy, fractures and more.
Infant Breathing Problems
Infants are much more likely to experience breathing problems if they are delivered via C-section. It is important that babies are constantly monitored after birth as breathing problems may lead to respiratory distress syndrome and long-term health problems.
Prognosis for C-Section Injuries and Birth Injuries
C-section injuries are relatively uncommon, but they do happen. If injuries are recognized quickly and treatment is initiated, the prognosis after a C-section injury is generally good. It is important to follow your doctor’s instructions while recovering in order to reduce the likelihood of additional complications.
In terms of c-section injuries and birth injuries, the prognosis will depend on the type of injury and the severity. For example, fetal lacerations may heal rather quickly and may even resolve without scarring. However, a more substantial injury like brain damage or cerebral palsy may never completely resolve, leading to a more challenging prognosis. What is most important in these situations is to build, and work together with, a team of healthcare providers across specialties that can help develop a life care plan for your child. This plan should include immediate and ongoing medical concerns, treatment options, costs, and so on. A well-developed life care plan can help parents and healthcare providers understand the child’s current situation and make the best decisions possible about their ongoing care.
Getting Help After a Birth Injury
If you or your child is suffering from a birth injury, you should know that help is available. As a patient, you have the right to receive quality care that meets accepted medical standards. If a healthcare provider or facility fails to do so, you may have grounds to file a medical negligence claim. The best way to learn more about your legal rights and possible options to recover from a birth injury is to contact a birth injury lawyer.
At Birth Injury Guide, our team has extensive experience helping clients sort out the details of birth injuries and their aftermath. Contact us to learn more, or to speak with a birth injury lawyer. Our consultations are always free, and you are under no obligation by contacting us. You can also learn more by visiting our Birth Injury FAQ page.
Start Your FREE Case Review Today
If you or your child is injured as a result of medical negligence, call us to learn more.



