
Infant Cephalohematoma
Infant cephalohematoma is a medical condition that occurs in 1-2 percent of all live births. This condition is more likely to happen if birth-assisting tools are used during delivery; such as forceps or vacuum extraction. If forceps or a vacuum were used; the rate of cephalohematoma increases to 3-4 percent. Improper use of birth-assisting tools is a type of birth injury that may also be considered medical negligence.
Although it is considered a minor injury; that usually heals without any major medical problems, there are certain factors related to cephalohematoma that may lead to additional complications.
What is Infant Cephalohematoma?
What is cephalohematoma? Cephalohematoma is a traumatic subperiosteal hematoma that occurs underneath the skin, above the periosteum of the infant’s skull. The periosteum is a layer of connective tissue that surrounds the skull bone. A newborn’s blood vessels are incredibly vulnerable. Pressure on the head during delivery can cause these blood vessels to rupture, which causes blood to pool up. The exact location of cephalohematoma in newborns varies depending on where on the baby’s head the ruptured blood vessels are. This further depends on how the baby is positioned and where the pressure is applied.
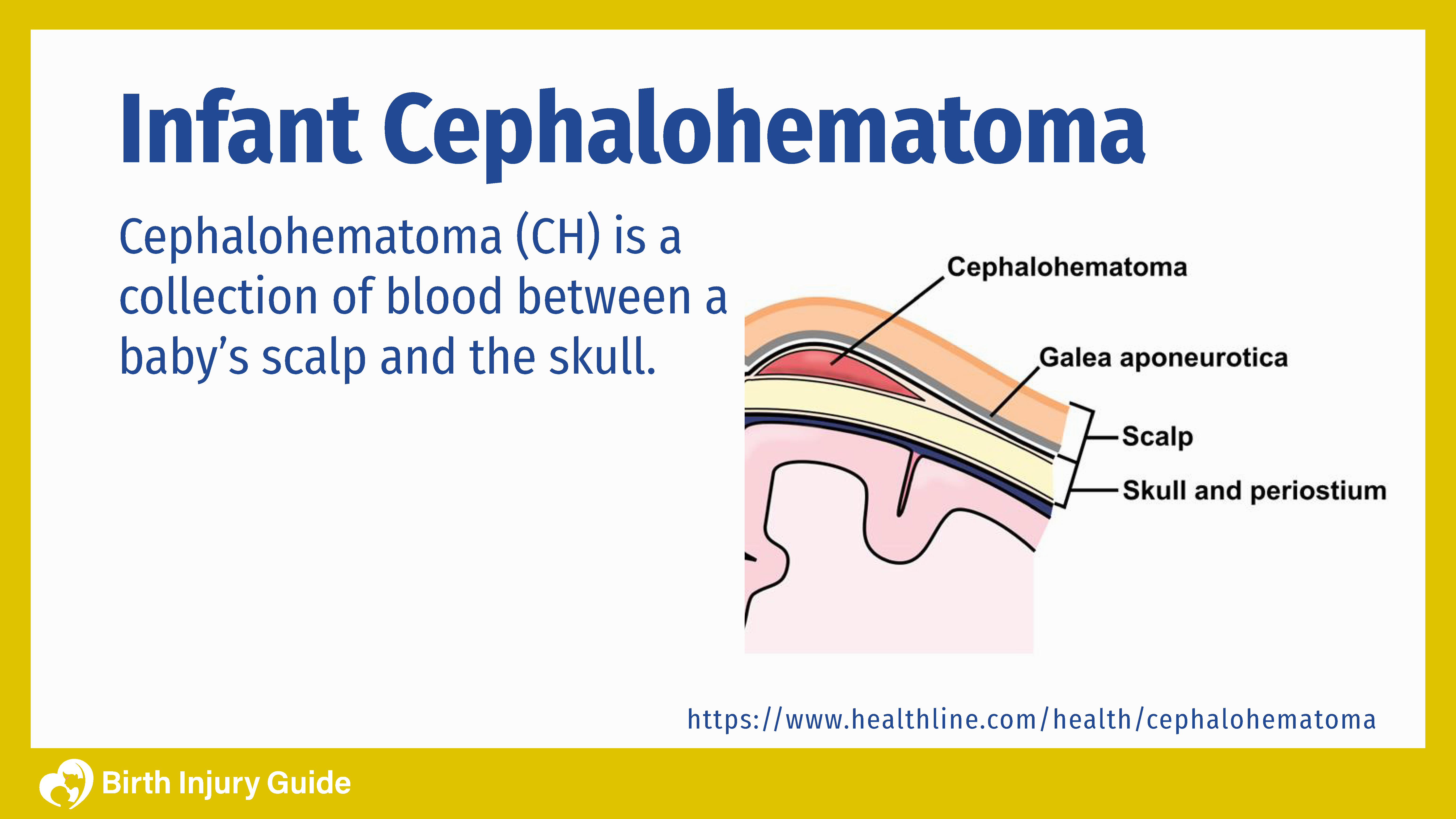
Cephalohematoma does not pose any risk to brain cells, but it causes unnecessary pooling of blood from damaged blood vessels between the skull and inner layers of the skin. Cephalohematomas are not usually evident at birth but develop during the hours and days following birth due to the gradual nature of the blood accumulation.
Causes
Cephalohematoma is a birth injury that occurs during labor and delivery. Any baby that is delivered vaginally can experience this injury. It often occurs as a result of difficult or prolonged labor as the baby moves through the birth canal. Sometimes the infant’s is hit against the mothers pelvic bone during delivery, which can rupture blood vessels. Other times, the birth canal is narrow and tight, which puts pressure on the infant’s skull that can also cause blood vessels to rupture.
In addition, medical research links the use of forceps during delivery with a heightened risk of Cephalohematoma. This is especially true when the healthcare provider applies excessive force to the infant’s head to pull him or her through the birth canal. There is also some evidence that cephalohematoma is more common in babies born to mothers who received an epidural. Because an epidural numbs the lower body, the mother is unable to push as effectively as she could during natural birth. This can create a more difficult or prolonged labor, which increases the risk for cephalohematoma.
Is There A Way To Prevent It?
The best way to prevent cephalohematoma is to recognize possible risk factors and adjust prenatal care accordingly. Some of the primary risk factors for cephalohematoma include:
- Fetal Macrosomia: A medical term indicating that the baby’s head is larger than the mother’s pelvic area. The larger the baby is, the more difficult labor can become. Baby’s with macrosomia generally weigh more than nine pounds.
- Weak or ineffective uterine contractions
- Difficult, prolonged labor
- Abnormal fetal presentation
- Multiples
What are the Symptoms of Infant Cephalohematoma?
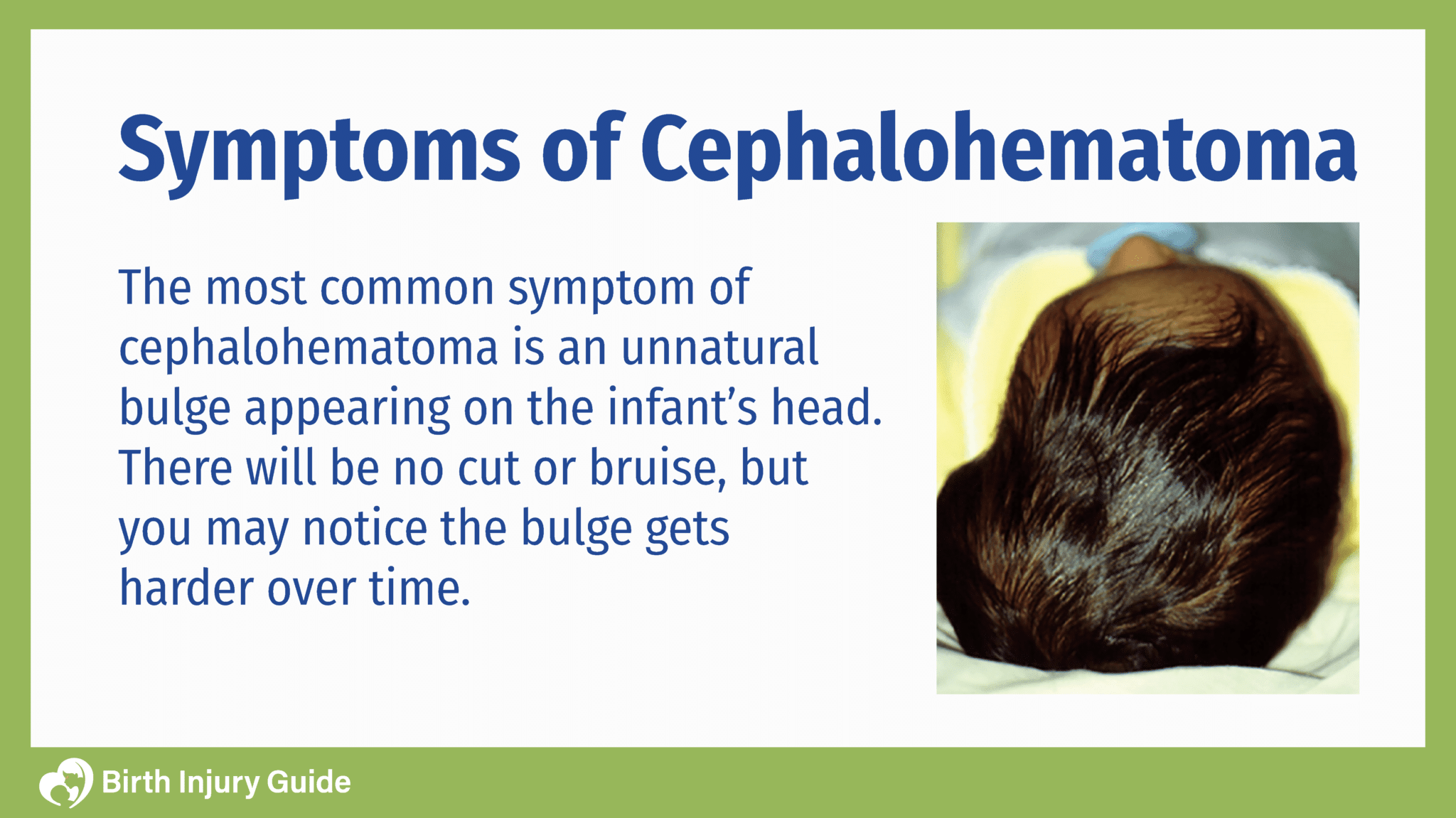
Cephalohematoma is mostly internal, so it’s not as easy to see as a laceration, and newborns may not react with obvious behavioral symptoms.
Less common, but relevant symptoms that a doctor can diagnose include:
- Anemia
- Infection
- Jaundice
If you find an unnatural bulge on the baby’s head; your physician should check it out immediately.
Diagnosis
The first and most important step is: to get your baby examined by a doctor. Your doctor can guide you on the best way to handle your child’s cephalohematoma. Some cases require treatment, and others resolve on their own over time.
To diagnose cephalohematoma, your doctor will perform a thorough medical examination. The appearance of a bulge on your baby’s head may be enough to make a diagnosis, but your doctor may order additional tests before confirming the diagnosis. Additional tests that your doctor may order include:
- X-ray: Uses ionizing radiation to produce images of the bones and other internal structures. X-rays are painless and quick tests.
- CT scan: Uses ionizing radiation to produce cross-sections of the inside of the body. CT scans include images of bones, soft tissue and blood vessels. They are quick and painless tests.
- MRI: Uses magnetic waves to product images of tissue and organs inside the body. MRIs are painless, but do require around 45 minutes, which can be distressing for some people.
- Ultrasound: Uses sound waves to produce images of organs and internal structures of the body. It is also the device used to view and monitor infants during pregnancy.
Imaging tests will show your doctor if there are any other problems, which will allow him or her to confirm cephalohematoma or make another diagnosis. In either case, this allows your doctor to get a better overall picture of your child’s health.
Treatment
In most instances, babies don’t require much treatment of cephalohematoma. infants will heal on their own within three months. However, hardening of the hematoma can occur causing significant deformities of the skull. This occurs because the blood calcifies and the area becomes harder. Sometimes, as the blood disappears, the baby’s skull may have a crater-like appearance where the bulge used to be. When a cephalohematoma is calcified, it can be alarming to parents.
In addition to deformity, other complications include infection that can lead to sepsis or osteomyelitis. These complications are very rare, but you should be aware that they can happen.
In cases where the blood build-up is so excessive that it lowers the baby’s red blood cell count, a blood transfusion may become necessary.
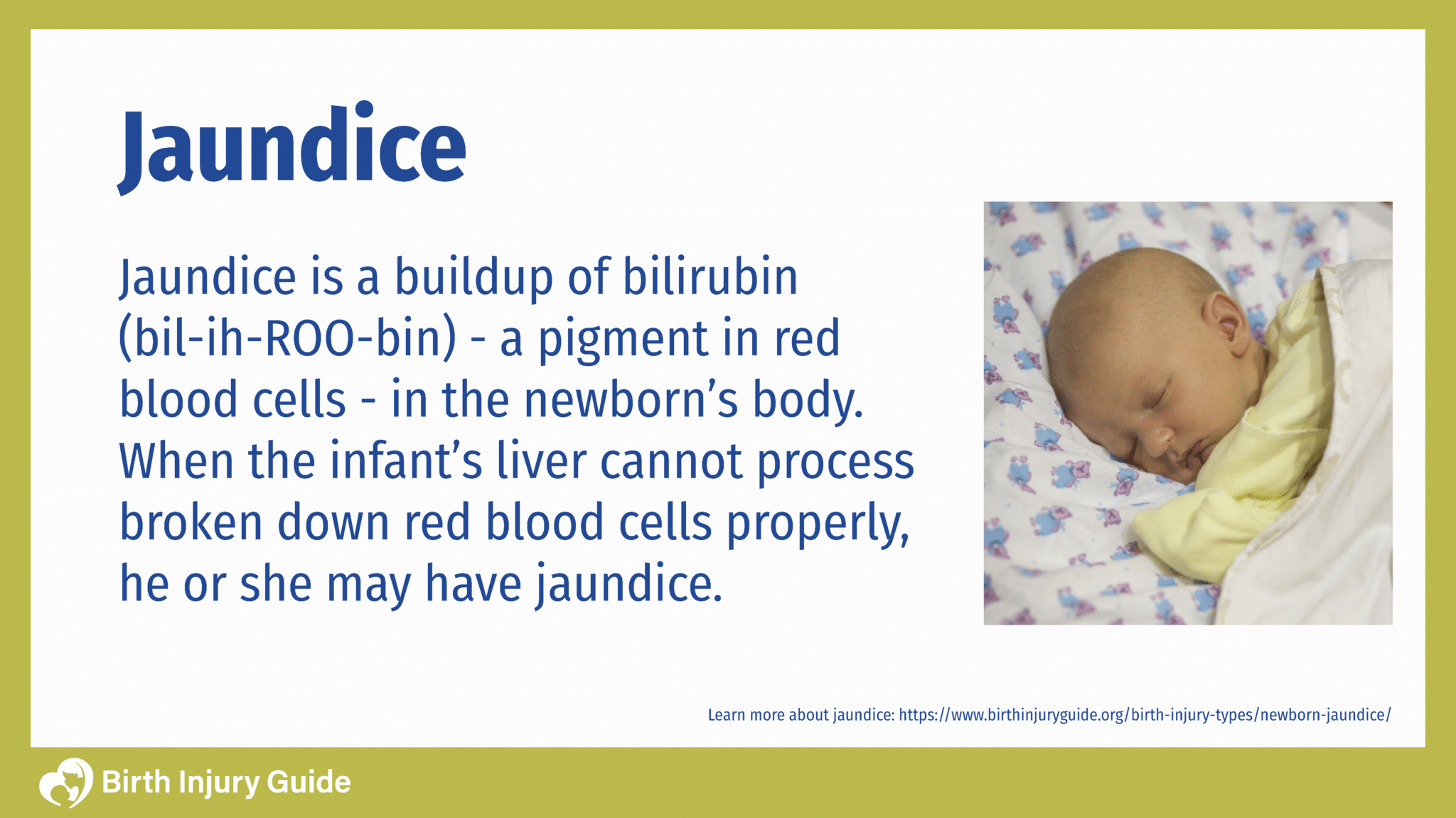
Cephalohematoma vs. Jaundice
Infants with cephalohematoma are also at a heightened risk for developing jaundice, because as the blood cells break down the levels of bilirubin increase. In these instances, and if the bilirubin is excessively high, cephalohematoma treatment may include phototherapy.
Infant Cephalohematoma Healing Time
Although most infants with cephalohematoma will heal on their own, it’s important to monitor and observe your child. Keep a close eye on any additional bulging or signs of jaundice. Also, keep an eye out for behavioral changes.

As long as your child is healing, the prognosis for cephalohematoma is generally very good. The key is keeping your healthcare provider informed of any changes in your child’s health or behavior. It also helps to be aware of possible risk factors and complications. Every child is different, so it’s important to remember to focus on your child’s health and prognosis based on his or her overall health.
Prognosis for Infants with Cephalohematoma
The prognosis for infants with cephalohematoma is generally very good. Most infants recover without complications. However, there are some cephalohematoma complications that can affect your child long-term. One of those complications is anemia. Cephalohematoma can cause your baby to experience anemia, possibly requiring a blood transfusion. Because blood builds up in one area, red blood counts (levels) can drop. Boosting red blood cells can improve the symptoms of anemia.
The other complication that may result from cephalohematoma is jaundice. Jaundice is a common medical condition that many newborns experience. It is incredibly important that jaundice be recognized and treated in a timely manner, however. Without adequate treatment, jaundice can lead to kernicterus, a dangerous type of brain damage. This is a complication that can dramatically impact your child’s prognosis. Brain damage from kernicterus can lead to lifelong disorders like cerebral palsy.
As you can see, your child’s prognosis largely depends on his or her overall health, development of complications and how well they respond to treatment. The key to a positive prognosis and outcome is adequate recognition, treatment and/or monitoring of cephalohematoma.
Start Your FREE Case Review Today
If you or your child is injured as a result of medical negligence, call us to learn more.



