
Report Reviews Neuroimaging Studies among Preterm Infants
A new report from the American Academy of Pediatrics (AAP) reviews neuroimaging practices among preterm infants. Neuroimaging studies are often used in the neonatal intensive care unit (NICU) to monitor preterm infants and aid in diagnostics, therapies and prognosis. Studies help doctors identify infants with brain injuries who may need interventions or who may be at risk for Neurodevelopmental impairment.
The report from the AAP was developed by the Committee on Fetus and Newborn, Section on Neurology and Section on Radiology. Titled, “Routine Neuroimaging of the Preterm Brain”, the report summarizes general methods of imaging, optimal timing for studies and the prognostic value of neuroimaging.
Preterm Infants At Risk for Brain Injuries
Preterm infants born before 30 weeks gestation, are at a significantly higher risk of experiencing brain hemorrhages or injuries to the white matter of the brain. The more premature the infant is, the greater the risk becomes. Preterm infants born after 30 weeks are less likely to suffer severe brain injuries unless there are additional risk factors.
The primary risk for preterm infants is intraventricular hemorrhage (IVH). This is bleeding that occurs inside or near the ventricles in the brain. The ventricles are spaces in the brain that hold cerebral spinal fluid.
Information about IVH
A premature baby brain bleed, such as IVH, can put pressure on the nerve cells in the brain and cause damage. Severe damage can cause brain injury. Because there are various degrees of severity, healthcare providers use a system of grading IVH depending on the amount of bleeding that is occurring. These grades are:
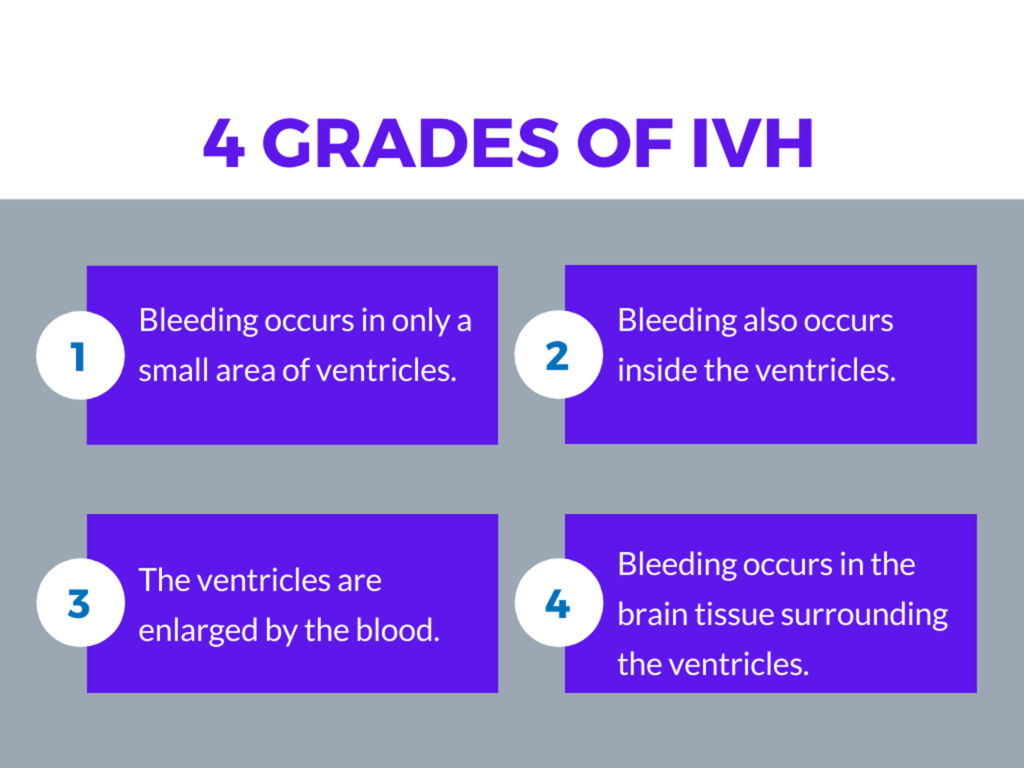
Grades one and two are the most common, and generally involve no other complications. Grades three and four are the most serious, and can result in long-term brain damage.
Most cases of IVH happen within the first three days of life. Therefore, it is recommended that healthcare providers screen for brain injury within 7-10 days. Healthcare providers may use various screening options, such as sequential cranial ultrasonography, which identifies lesions associated with cerebral palsy.
Imaging Techniques
The AAP report identifies computerized tomography (CT) scans as the traditional method of screening for preterm infant brain damage. However, it is no longer recommended due to the risk of radiation exposure. Now, cranial ultrasonographic imaging is the preferred imaging method.
Ultrasonographic imaging provides views from the anterior (near the front) and mastoid (near the back) fontanelles. These views can help identify cerebellar hemorrhage. Significant hemorrhage occurs in up to 9% of preterm infants, so better identification methods are important.
Another imaging method that is increasingly used for preterm infants is magnetic resonance imaging (MRI). An MRI can identify a brain injury and provide a detailed image of the brain. It is often preferred because an MRI does not use radiation like a CT scan. MRI studies may be used in preterm infants who are term-equivalent in age. Often, they do not require sedation.
Recommendations for Preterm Infants
Since IVH is more common in preterm infants, and can be significant, adequate identification and intervention is crucial to prevent permanent or serious brain damage. To that end, the AAP Committee on Fetus and Newborn offers the following recommendations:
- Infants born at or before 30 weeks gestation who are at an increased risk for injury should be screened for IVH with cranial ultrasonography.
- Routine cranial ultrasonography is recommended within 7-10 days of birth for infants born before 30 weeks gestation.
- Screening for IVH before 7 days may be recommended if the infant has symptoms of brain injury. In such cases, screening should be repeated at 4-6 weeks old, and at term-equivalent age.
- Preterm infants who have an abnormal cranial ultrasonography finding should have repeat screenings based on gestational and chronologic age.
- Standard cranial ultrasonographic imaging should include views from anterior and mastoid fontanelles. For additional information, posterior fontanelle imaging should be performed.
- CT scans are no longer a preferred or standard imaging method for preterm infant brains.
- MRIs are not a routine procedure for preterm infants, however they are useful at term-equivalent age for high-risk infants.
These recommendations are based on the consideration that NICUs use different routines and methods for screening. Appropriate timing and imaging method can help identify infants with brain injuries and initiate interventions as soon as possible.

