
Fetal Lacerations
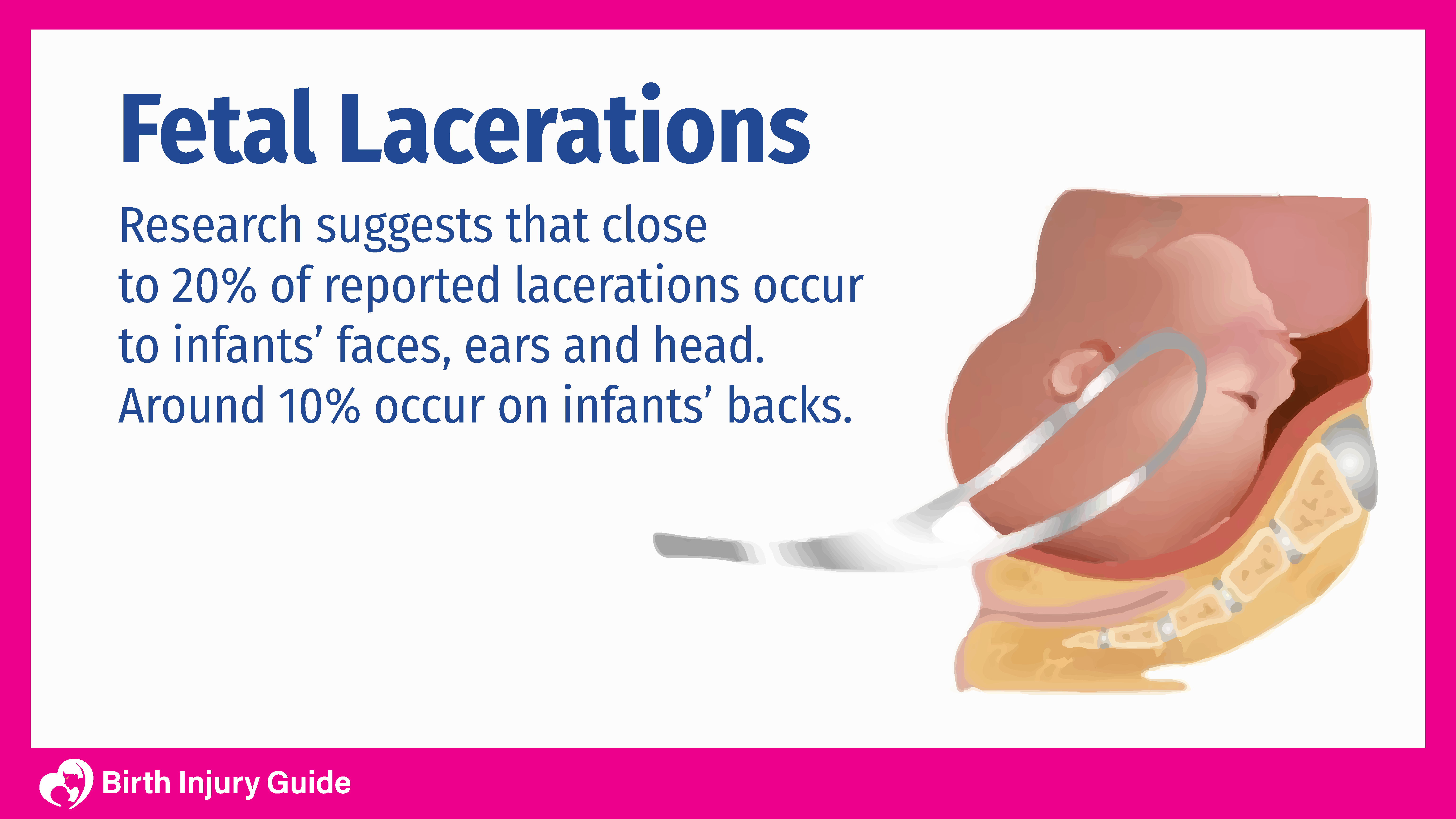
Fetal lacerations are birth injuries that occur during a Caesarean section (C-section) delivery, usually as a result of improper use of birth assisting tools. Lacerations are often caused by scalpels, forceps and other instruments used by physicians during labor or delivery. Generally, lacerations are minor and easily treatable. In some cases, however, they can be deep and require stitches or even reconstructive surgery.
What are Fetal Lacerations?
Fetal lacerations are cuts that occur during delivery. Most often, lacerations occur during C-section deliveries as doctors use scalpels and other sharp instruments to deliver the infant. Most of these injuries occur to the ears, face and head.
Per the Patient Safety Authority (PSA), a study of close to 900 women who underwent C-sections showed that between 1.5 percent to 1.9 percent of infants experienced fetal lacerations. However, another similar study showed that the rate of injury is closer to six percent. In yet another study, the National Institutes of Health (NIH) states that these injuries occur in at least three percent of all pregnancies.
One reason that the results may vary is because of an increase in C-sections. Regardless, fetal lacerations can be problematic, and sometimes, can contribute to long-term injuries.
What Causes Fetal Lacerations?
There are several risk factors that increase the chances for fetal lacerations occurring during a C-section delivery. The principal risk factors include:
- Ruptured membranes before the C-section
- Low transverse uterine incisions
- Active labor
- Emergency C-section
- Inexperienced surgeons or residents
- Needing to cut through the placenta to get to the baby
- Undeveloped lower uterine segment (a uterus that has not labored)
Can Fetal Lacerations be Prevented?
There is ongoing research looking for possible ways to prevent fetal lacerations. Although research continues, a device called CSafe has proven to be an effective method. The CSafe is a small surgical tool that offers added protection during the C-section process by allowing physicians to cut upwards and away from the infant.
Other prevention strategies include:
- Moving the uterine wall prior to incision.
- Elevating the presenting part – pushing it away from the incision manually by pushing on the outer uterine wall overlying the head, buttocks if the baby is breech, or the back if the baby is transverse.
- Blunt entry into the uterine cavity prior to incision.
- Using bandaged scissors.
- Removing abdominal wall retractors prior to incision.
Start Your FREE Case Review Today
If you or your child is injured as a result of medical negligence, call us to learn more.
Fetal Laceration Symptoms
The most common symptom of a fetal laceration is a cut or open wound. That is not the only symptom that a newborn may experience, however. Other symptoms may include:
Bone Fractures
Bone fractures occur in eight out of every 1,000 births that include fetal lacerations, according to the National Institute of Child Health and Human Development. Cranial injuries, specifically cephalohematoma, occurs in at least 272 out of 1,000 births that include fetal lacerations.
Viral or Bacterial Infections
If an infant suffers a laceration during delivery, he or she may be vulnerable to maternal infections. Maternal infections like Group B Strep live inside the vagina and can be passed to the infant during delivery. An open cut on the infant during delivery increases the risk of an infection.
Tendon Injuries
Tendons can also be injured if an infant suffers a laceration. Tendons are made of tissue that connect muscles to bone. If a laceration is deep enough, it can damage the tendons.
Facial Nerve Palsy
If a laceration occurs on the infant’s face, the affected facial nerves may become paralyzed. Fetal lacerations and bone fractures can both cause facial nerve palsy.
Fetal Laceration Treatment
Treatment of fetal lacerations will depend on how deep and long the cut is, as well as any other injuries or medical conditions present. For minor cuts, physicians often prefer to apply topical tissue adhesives to the wound. For more severe lacerations, physicians may perform suturing, meaning the cut is stitched up using a suture medical device.
In addition to closing the wound, oral antibiotics may be prescribed to treat any infection present, or to prevent an infection from occurring.
Prognosis for Fetal Lacerations
Generally, the prognosis for fetal lacerations is favorable. With timely treatment and monitoring for possible infections or complications, most infants recover without incident. Infants who develop facial nerve palsy or have more severe injuries may require a longer treatment program or reconstructive surgery, but still, the prognosis is generally positive.



